Selling Your Hospital, Part 2
This post was originally published on the California Society of Anesthesiologist’s (CSA) webpage on March 7, 2016 With their website rebuild, the archives were not posted.
Home » CSA Online First » Christine Doyle » Selling Your Hospital, Part 2
Selling Your Hospital, Part 2
Mar 07, 2016 by Christine Doyle, M.D.
tags: hospitals

Between the initial announcement of the DCHS sale in October 2014, the conditional approval by the Attorney General on February 20, 2015, and Prime’s withdrawal of its offer on March 10, 2015, we held many meetings. Prime’s operations team visited on several occasions to review our processes and make suggestions. We started implementing some of them immediately, and others later.
 Probably the most important factor that changed was our attitude. We learned how truly important our documentation was for the hospital’s ability to bill for services. We learned about how coders do their work, even if we will never actually do it, so that we could help make their jobs easier. Our medical staff president spent hours one-on-one with our admitting physicians, showing them the difference a single word could make. Most of us had no idea, for example, that “urosepsis” wasn’t a valid diagnosis according to CMS. This information brought secondary benefits as well, as the ICD-10 transition became a non-issue for us.
Probably the most important factor that changed was our attitude. We learned how truly important our documentation was for the hospital’s ability to bill for services. We learned about how coders do their work, even if we will never actually do it, so that we could help make their jobs easier. Our medical staff president spent hours one-on-one with our admitting physicians, showing them the difference a single word could make. Most of us had no idea, for example, that “urosepsis” wasn’t a valid diagnosis according to CMS. This information brought secondary benefits as well, as the ICD-10 transition became a non-issue for us.
Our Geometric Mean Length of Stay (GMLOS), which started out 1.5 days over the target, was reduced to 0.1 days over the target within nine months. Although the actual increase in revenue was not known to us, it was clear that we were appropriately aligning our documentation with what was required by CMS.
We also looked long and hard at our expenses. A mitigation plan, aimed to reduce those expenses, was enacted in April. It was not without controversy, nor was it without revision. Key issues included inaccurate job titles, descriptions, and an overemphasis on confidentiality, leading to crucial positions being eliminated (i.e., our surgery biller) only to be subsequently reinstated. Low-volume service lines were closed or reconfigured.
Communication, once again, became a critically important part of the process. Rumors flew amongst the hospital staff, the local news, patients, other hospitals, and neighbors. Damage control again became important, especially since early advertising had been all about how the hospitals would close if the sale fell through. Fortunately, cash flow improved with receipt of deposit money from Prime and additional state funds.
DCHS filed suit against SEIU and Blue Wolf in Superior Court. Among the complaints were breach of contract for violating the confidentiality clauses, unfair competition by discouraging potential bidders, civil conspiracy for taking action that caused harm to DCHS, and aiding and abetting when Blue Wolf allowed SEIU to influence competing bidders.*
In response, the Attorney General’s office issued this press release, blaming Prime for breaking the deal. Her comments raised concerns that the conditions placed on any other sale would be the same or even more restrictive. These concerns were only slightly appeased when Attorney General Harris stated that “the offer made to Prime was unique and tailored to Prime,” and that conditions for a different transaction would not necessarily be the same.
 Back to square 1 (or maybe 2).
Back to square 1 (or maybe 2).
Within two weeks of the announcement that Prime refused the deal with the Attorney General’s conditions, our agents were again fielding requests from interested parties. The process was the same as before, so much of the work was already done. Our financial situation had slightly improved, and we updated the prospectus. Once again, we engaged in discussions with the Attorney General’s office, and with officials in Paris and Rome, so that when we had a potential buyer we would be able to move in an expedited fashion.
My mother and her neighbors who live within half a mile of the hospital sent letters to Santa Clara Supervisor Ken Yeager and San Jose Councilman Pierluigi Oliverio. They emphasized that the county would suffer a decline in tax revenue and other negative financial implications if businesses (physician offices) moved away from the area when O’Connor became “Valley North.” They asserted that property values would decline in one of the oldest, exclusive neighborhoods in San Jose. No response was received, and both Yeager and Oliverio remained remarkably silent on the entire situation.
The selection committee was reconstituted, with the addition of Sister Margaret Keaveney, who had been named the CEO of O’Connor Hospital after the planned departure of the prior CEO. It turned out that the original committee had no direct representation from the hospitals. Some observers felt that such representation might have improved the bid process and timeline.
After mostly behind-the-scenes machinations, an announcement was made on July 17, 2015, that the selected buyer would be Blue Mountain Capital in conjunction with Integrity Healthcare. The former would provide the capital and the latter the management. Key provisions of the plan included maintaining the hospitals as non-profits for at least three years, keeping them open for at least five years, and conversion of the “church plan” retirement fund to an ERISA-compliant fund.
Both parties had been involved in the original bid. Integrity had been one of the finalists, but had been unable to secure funding in a timely manner. This new combination afforded each the opportunity to play to their strengths. The management team, with whom we would be working, was comprised of executives with extensive experience in California managing both community and academic hospitals.
The paperwork was submitted to the Attorney General’s office on July 31. This meant that the 105th day allotted for public review landed on Friday, November 13. Open hearings were scheduled for the second week in October, and they were much shorter and less contentious. SEIU was remarkably quiet. The final announcement from the Attorney General’s office was made, after a short extension, on December 3. The conditions were as expected, and were accepted by Blue Mountain/Integrity.

On December 14 at 10 am, the formal transfer took place, and we became Verity Healthcare.
______________________________
*Media references to the lawsuit:
http://sternburgerwithfries.blogspot.com/2015/03/seiu-uhws-dave-regan-and-blue-wolf.html
http://www.modernhealthcare.com/article/20150225/NEWS/150229929
http://www.wsj.com/articles/when-unions-trump-hospitals-1426721146
http://www.mercurynews.com/news/ci_29250106/daughters-of-charity-health-system-closes-deal-with-hedge-fund
Selling Your Hospital, Part 1
This post was originally published on the California Society of Anesthesiologist’s (CSA) webpage on 2/29/2016. With their website rebuild, the archives were not posted.
Home » CSA Online First » Christine Doyle » Selling Your Hospital, Part 1
Selling Your Hospital, Part 1
Feb 29, 2016 by Christine Doyle, M.D.
tags: hospitals

My anesthesiology group practices at one of the Daughters of Charity Health Systems (DCHS) hospitals, and our members have been working there for over 30 years. In January 2014, the DCHS board announced a search for a buyer for the five hospitals and associated facilities.

Needless to say, everyone was flabbergasted, although it wasn’t news that our health care system was in trouble. Each facility has a significant proportion of patients who are covered by Medi-Cal, although not all of them reached a sufficient percentage to qualify as a “Disproportionate Share Hospital (DSH)” and receive DSH payment adjustment from CMS. The Daughters’ overarching goal of providing care to the poor and needy has tended to keep them running an operating loss budget, while investment revenue has declined to the point that it no longer offsets the losses.
Thus began a two-year rollercoaster process. While we often compare the process to selling a house, there are some significant differences to keep in mind about the process of selling a health system.
After making the decision to sell, and choosing a broker, you have to create a prospectus for your facility or system. This prospectus is made available to potential buyers. Your broker will then collect information from potential buyers, who may be interested in acquiring the entire system or only certain parts. You will have a series of site visits from bidders, and many meetings with hospital administrators and medical staff.
Once you select a bidder, you must get a series of approvals for the sale. As a Roman Catholic health system, DCHS requires approval of the sale by the head of the Daughters of Charity in Paris, and by Pope Francis in Rome. As a California health system, we also must have the approval of Kamala Harris, California’s Attorney General.
DCHS contracted with Houlihan Lokey, a global investment bank with extensive experience in brokering hospital sales. Representatives of the firm came to talk to the medical staff and explain the process. One of the first points they explained was that the names of all potential bidders would be kept private except to the individuals on the selection team, in part to avoid outside attempts to influence the process. The names of the other bidders would become public when DCHS announced the selected bidder. Houlihan Lokey expected this phase, including on-site visits and due-diligence research by both sides, to last about six months.

Simultaneously, we began working with the Attorney General’s office and with officials in Paris and Rome. We knew that there were likely to be political ramifications of the sale, but we had no idea what they might be.
One of the overarching goals was to sell the system intact, because breaking up the system would have significant financial implications for the three different retirement funds. A break-up of the system would force a conversion of the existing church pension plan, which wasn’t covered by federal laws, to an ERISA-compliant plan, at a projected cost of about $200 million. The Daughters were adamant about protecting these funds both for current and retired staff.
As the summer progressed and the timeline slipped a bit, we started to hear rumors that one of the bidders was Prime Healthcare Services. The Service Employees International Union (SEIU) immediately contacted the ancillary hospital staff, urging them to oppose the deal. SEIU favored Blue Wolf Capital, a venture capital firm that had been co-founded by SEIU in 2005. The local newspaper printed a series of articles, reporting that the Santa Clara County Health & Hospital System (SCVHHS) wanted to buy O’Connor Hospital in San Jose and Saint Louise Regional Hospital in Gilroy, and that Prime was one of the competing bidders.
We kept hearing that the announcement would be made “soon.” It was finally made on October 10, 2015, as we were all traveling to New Orleans for the ASA Annual Meeting. Prime Healthcare’s bid was accepted at $843 million, in a mix of cash and specified capital investments.
Now the real work would begin.
As part of the requirement to submit the selected bid, as well as the other finalists’ bids, and supporting documents to the Attorney General’s office, the documents were made available online for public review. The documents for O’Connor Hospital alone filled 10 four-inch binders, which were available for a mandatory period of 105 days to anyone who wished to review them. There are also mandatory public hearings, and a site visit by a consultant appointed by the Attorney General’s office to make recommendations for conditions of the sale.
Make no bones about it, this was a POLITICAL decision, and like most political decisions, there were opinions and “spin” put forward by all sides.
The SEIU strongly opposed this deal unless Prime was willing to sign a “neutrality” agreement, which in union language means that the union may enter any facility and organize without any opposing action by management. Employees were divided, with most ultimately siding in favor of the sale.
The California Nurses Association (CNA) initially withheld judgment, but ultimately supported the deal as well. They felt that the sale provided the best option for their members, as it would preserve jobs and protect retirement funds.
Three of the five Santa Clara County Supervisors were vocally opposed to the deal. They serve as the Board of Directors for the county hospital system, which is constantly working at capacity, and acknowledged a clear bias in favor of a sale of the San Jose and Gilroy hospitals to the county.
 The local paper, the San Jose Mercury News, initially opposed the sale to Prime. Early on, SEIU published an invited commentary criticizing the deal, as did the Santa Clara county supervisors. Many people submitted letters to the editor, although only a few from the physicians and nurses were printed. Hospital staff encountered roadblocks in trying to contact the editorial board to tell the other side of the story. The hospital system’s advertisements implied the hospitals would all close immediately if the sale wasn’t approved.
The local paper, the San Jose Mercury News, initially opposed the sale to Prime. Early on, SEIU published an invited commentary criticizing the deal, as did the Santa Clara county supervisors. Many people submitted letters to the editor, although only a few from the physicians and nurses were printed. Hospital staff encountered roadblocks in trying to contact the editorial board to tell the other side of the story. The hospital system’s advertisements implied the hospitals would all close immediately if the sale wasn’t approved.
Public hearings were held the first week of January, nearly a year after the process started. Each facility was scheduled for a four-hour hearing, although all of them went on much longer. O’Connor’s lasted 11 hours! The Deputy Attorney General who was in charge had us sit on the “support” (right) side or “oppose” (left) side in the auditorium. SEIU sponsored a cadre of people who didn’t work at DCHS but who traveled and spoke against the sale at each hearing. One DCHS nurse wryly remarked, “I recognize most of the people sitting to my right, and I don’t recognize anyone sitting to my left.”
Given the sheer volume of documents as well as testimony to review, the Attorney General requested, and was later granted, a two-week extension. Her decision was announced at 5 pm on Friday, February 20. The decision was “Approve with Conditions” — 300 conditions in all. Some of the key provisions included a requirement to keep each of the facilities open as acute care hospitals for 10 years, keeping all current contracts, including some very unfavorable ones with two Medi-Cal HMOs. Another condition required increasing the amount of charity care provided each year, despite fewer people needing it, at least in theory, because of the Affordable Care Act.
Prime spent two weeks reviewing the conditions, and then announced on March 10 that they were withdrawing from the agreement because the conditions were onerous and would set a bad precedent.
Now what?
To be continued…
The Physician as Family Member
This post was originally published on the California Society of Anesthesiologist’s (CSA) webpage in 2012. With their website rebuild, the archives were not posted.
Home » CSA Online First » Christine Doyle » The Physician as Family Member
Nov 12, 2012 by Christine Doyle, M.D.
tags: anesthesiologist, Familiy, Patient

I call my mother to say my plane will be on time, and she tells me “someone” will pick me up, as they’re taking my uncle to the hospital with a BP of 220/120 and a HR of 40. Upon my arrival, I am whisked off to the local hospital’s ICU, where the neurosurgeon is assessing my uncle for surgery for his bilateral hygromas. I ask who the anesthesiologist will be and am told, “it doesn’t matter.”
Right, I think. Duly noted. Receiving the message that, as a patient, who your anesthesiologist is does not matter, really gave me something to think about. As someone who was considering my options for areas of specialty training in medicine, that message didn’t sit well with me. In addition, the comment made me feel uneasy about such an unfriendly, unengaging response to a concerned family member.
Flash forward 10 years. I’m on ICU call while doing my training in anesthesiology at Stanford and my pager goes off at 6:00 am. It’s my mother, telling me she’s taking my father to the ED of the same local hospital—the one where I will be starting on staff in 3 months—because “something is wrong.” I drive the 20 miles and meet them in the ED. We find that he has a ruptured spleen (from his thrombocytosis-induced splenomegaly), and will need surgery. The ED physicians ask who we want to see him, and luckily our first choice surgeon is on call. My future partner, Dr. Larry Sullivan, is the anesthesiologist on call, and I start to relax—just a bit.
I certainly knew by this time that who your anesthesiologist is does matter. I believed it so firmly I had selected it as my specialty. I was also more aware of the inner workings of the emergency medical setting and could assist my family better by asking tough questions and simplifying information.
Flash forward another 10 years. My cell phone rings, and I’m told my godmother is in the ED at my hospital with a stroke. I arrive in the ED, go to the back and the physician taking care of her (the “new guy” whom I haven’t met) says to me “Oh, I should have waited for you to intubate her.” I was glad I wasn’t faced with that option—I know that I can’t be objective in this situation. She has had a significant hemorrhagic stroke and may need surgery after we reverse her anticoagulation. The following day she does go to the OR for decompression. I knew everyone on the surgical team and was able to reassure the family members that she has great medical care.
Each of these experiences was stressful, but for different reasons. In the first, I knew the issues associated with increased ICP and the associated risks of anesthesia, but I didn’t know anyone involved in my uncle’s care, and was just “that surgery intern.” In the second, I was extremely stressed, but Dr. Sullivan made me relax by introducing me to the OR, PACU and ICU staff as “our new partner.” In the third, I was the one calming down everyone else, and confusing the staff as to my role in the ICU, since I was “just family.” It’s a tough and insightful experience to be a physician in the midst of a family medical emergency.
Medical school and residency do not always prepare us well with respect to patient/physician interactions. Simulated encounters, as used more often now, help physicians learn how to talk with patients and their families. As in all things, some of us are better than others. But none of us are taught how to deal with being the family member, or even the patient.
As a physician and specifically as an anesthesiologist, I have taken home several lessons from these various encounters. The first is that it’s much easier to talk with patients and family after you have been in those tough roles yourself—and they will recognize that empathy. The second is that “hello,” “please” and “thank you” go an awfully long way to making things better (just like I was taught in kindergarten). The third is that family members really need things to be explained in concrete terms (not the least of which is how you as an anesthesiologist are an important member of their care team). I found that the biggest thing I did was “translate,” not just from medical terms (which most of my extended family know, being in the business themselves), but to short declarative sentences. I frequently had to ask questions in a way that a short sentence was the only way to answer. And the last thing is that your colleagues will automatically look to you to function as the spokesperson, whether or not that’s appropriate. Be prepared to redirect your colleagues if necessary. Ask the difficult questions for the family members who won’t.
I know that I will be the family member again some day. And while I may be stressed and upset, my earlier experiences will make it easier for my colleagues and me to navigate the care of my loved ones in the future.
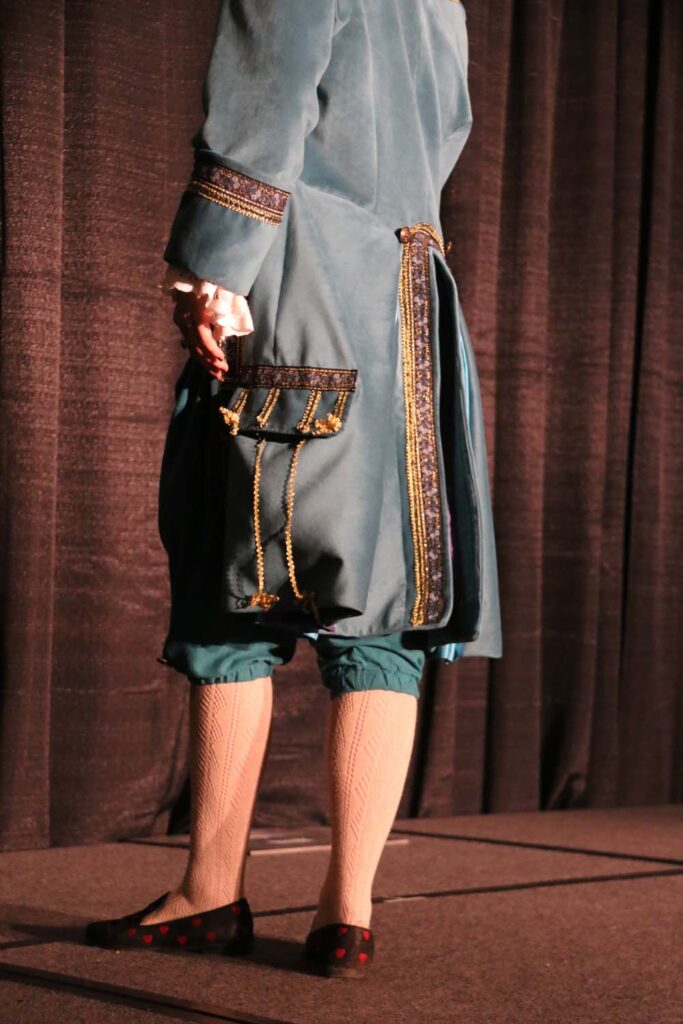
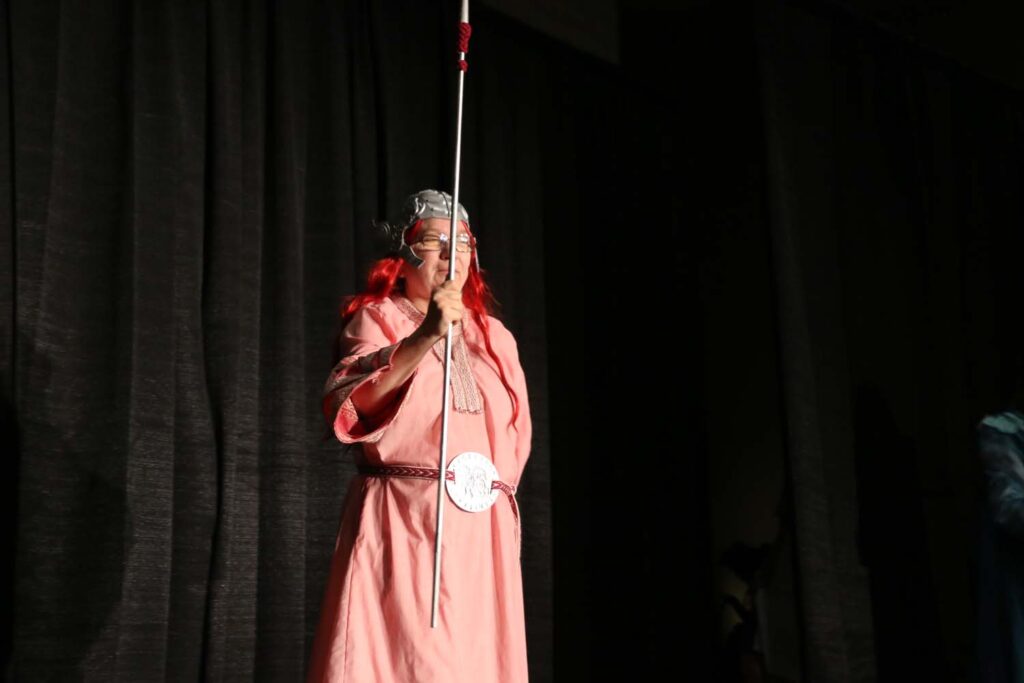
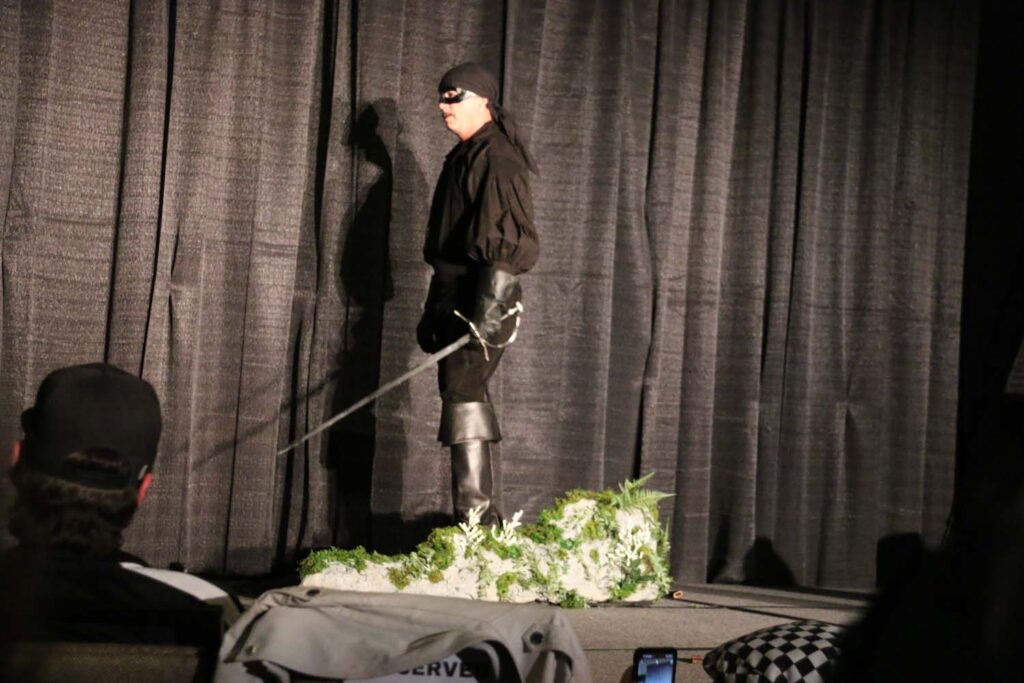
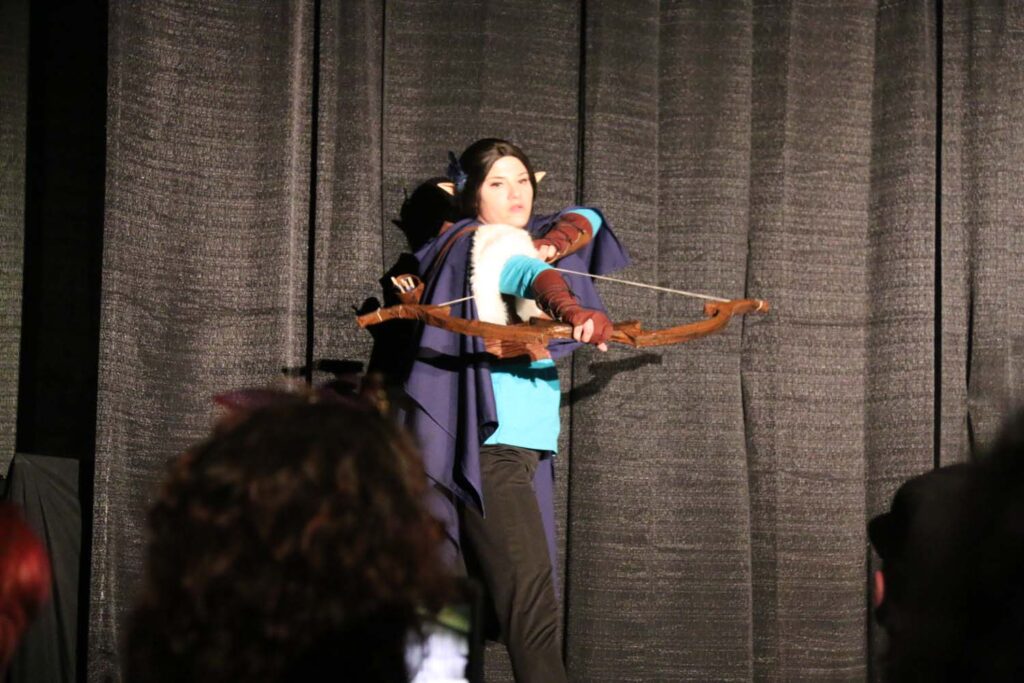
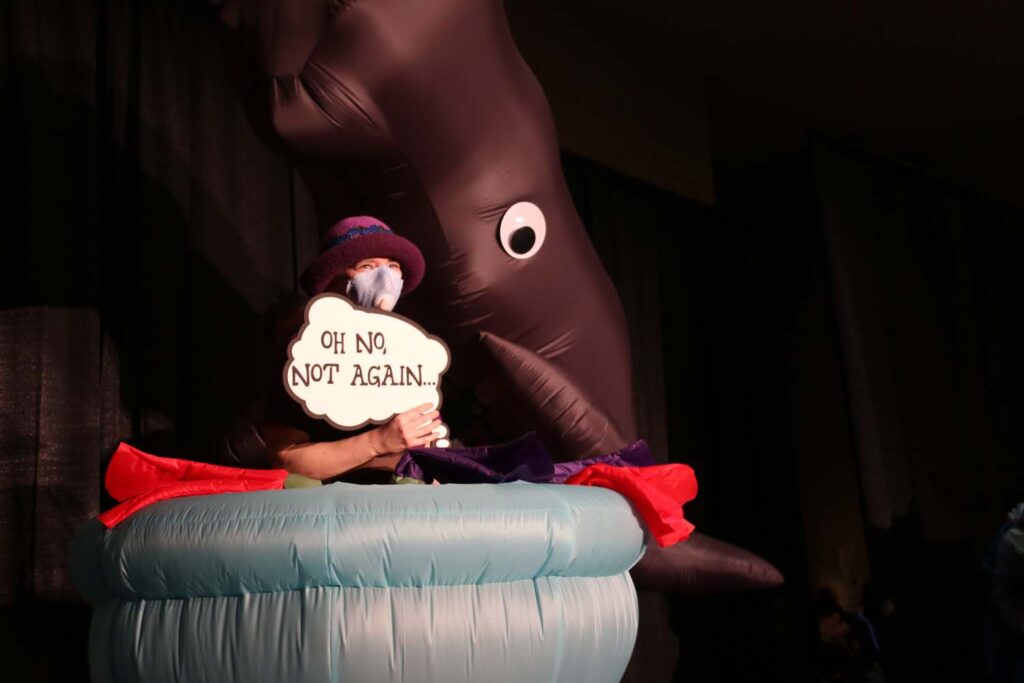
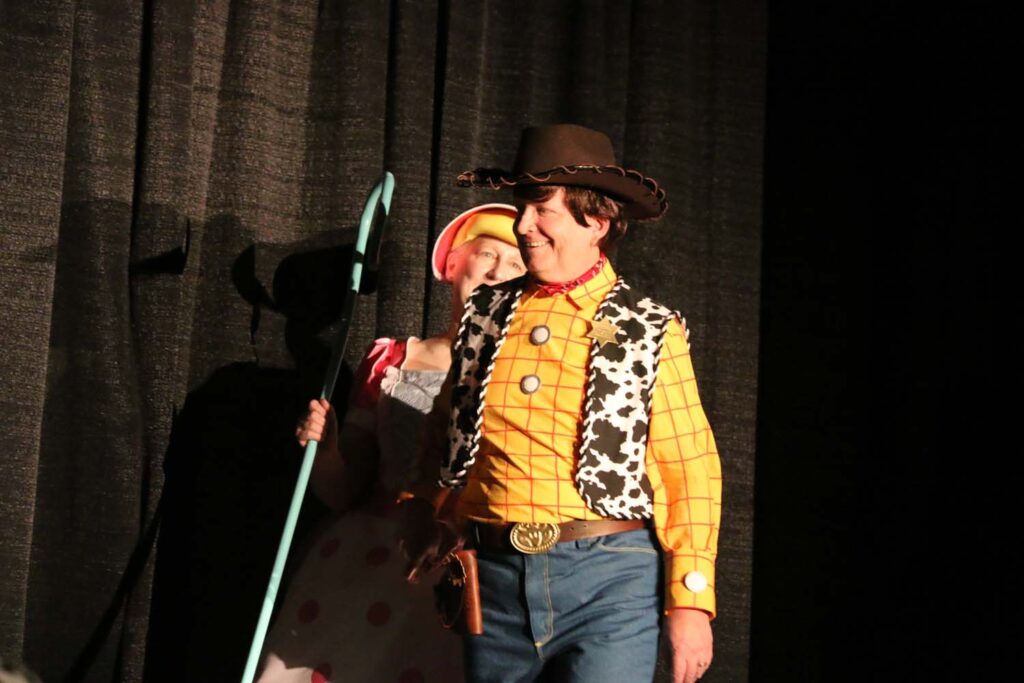
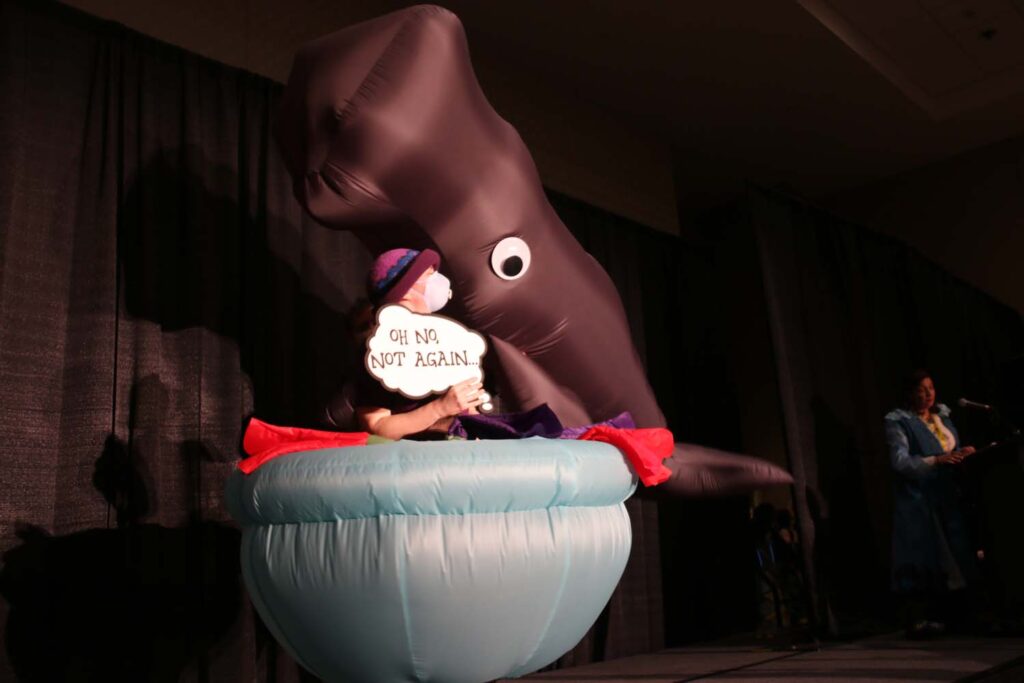
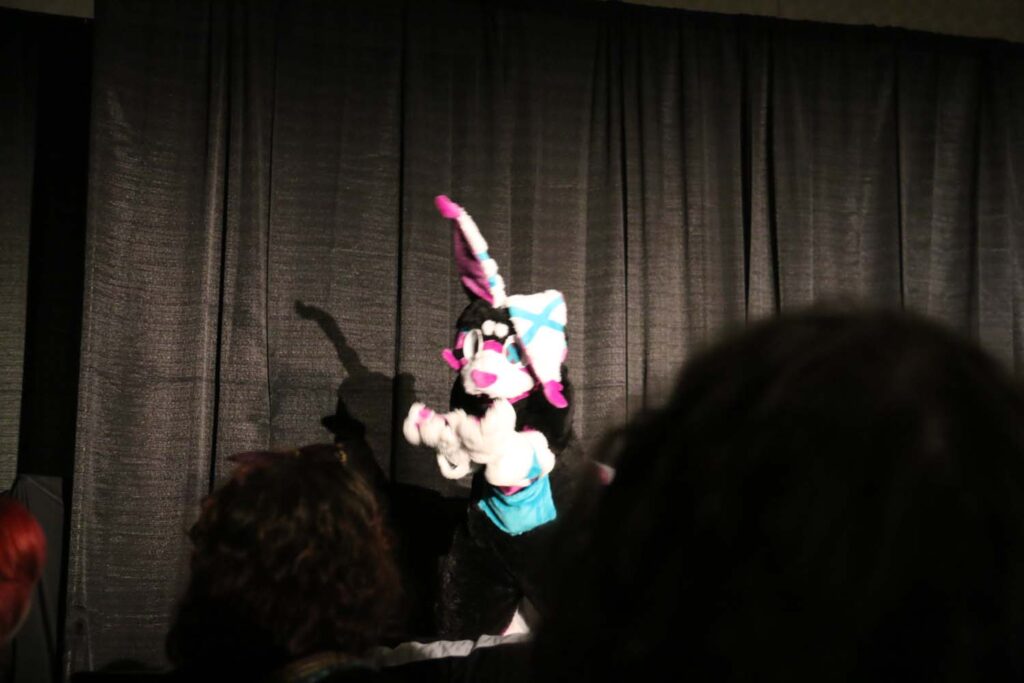
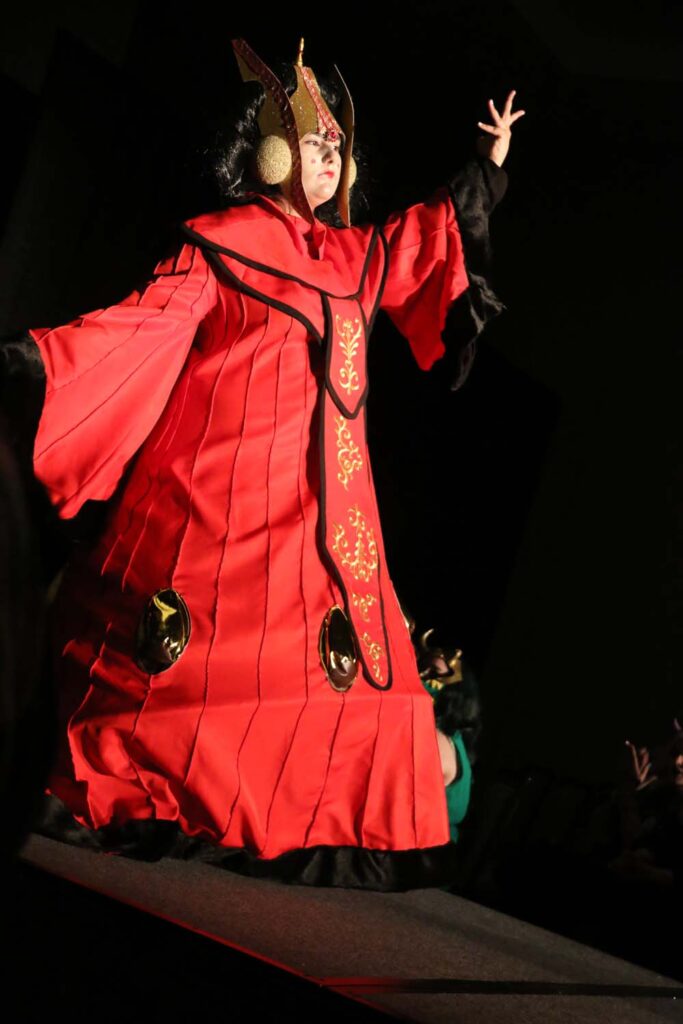
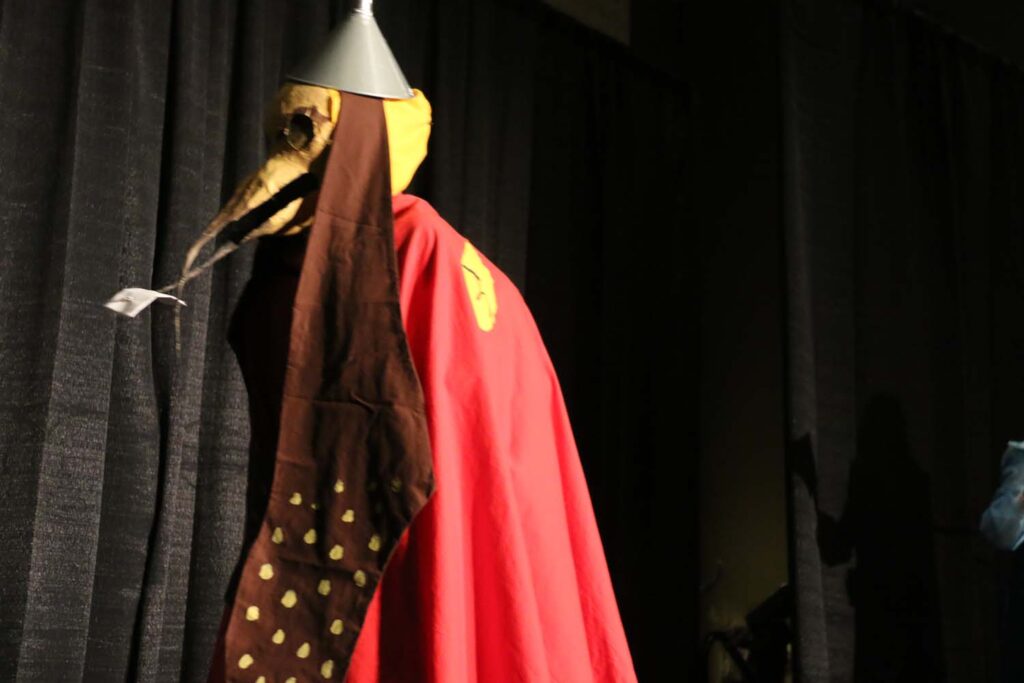
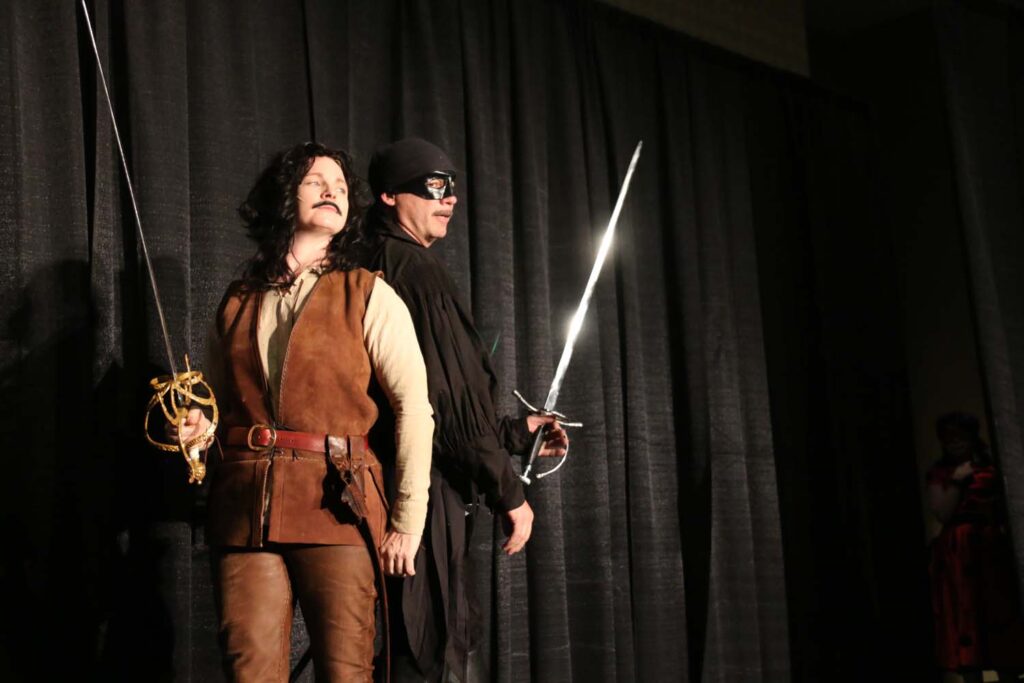
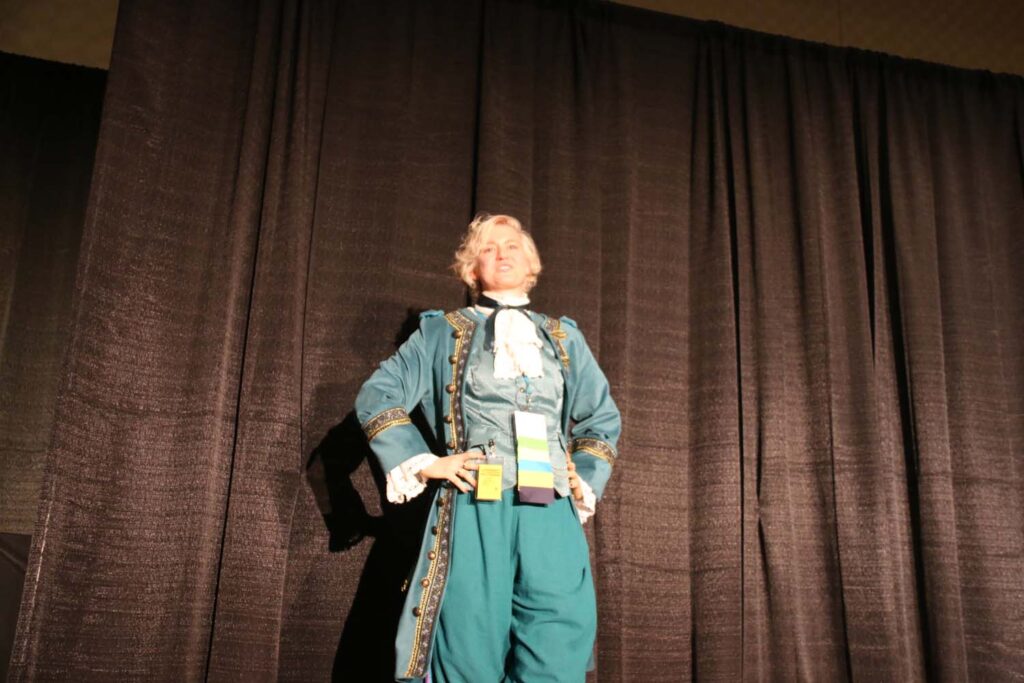
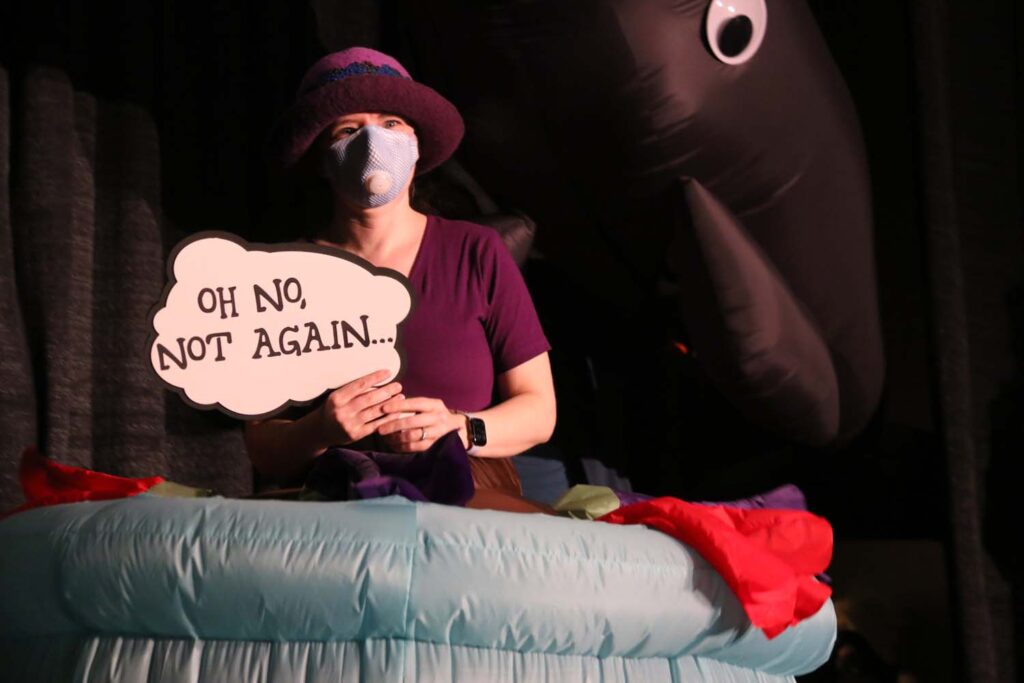
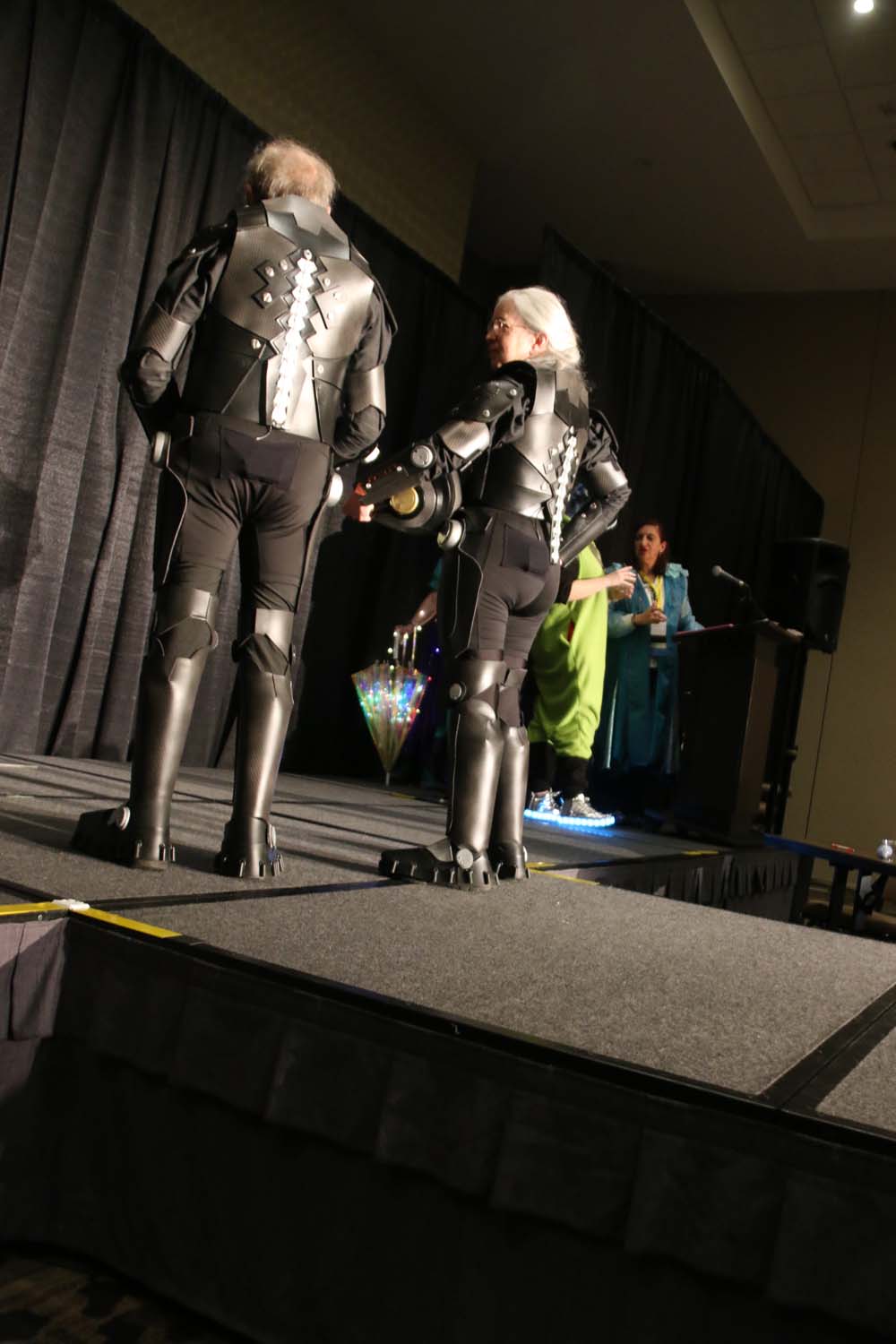
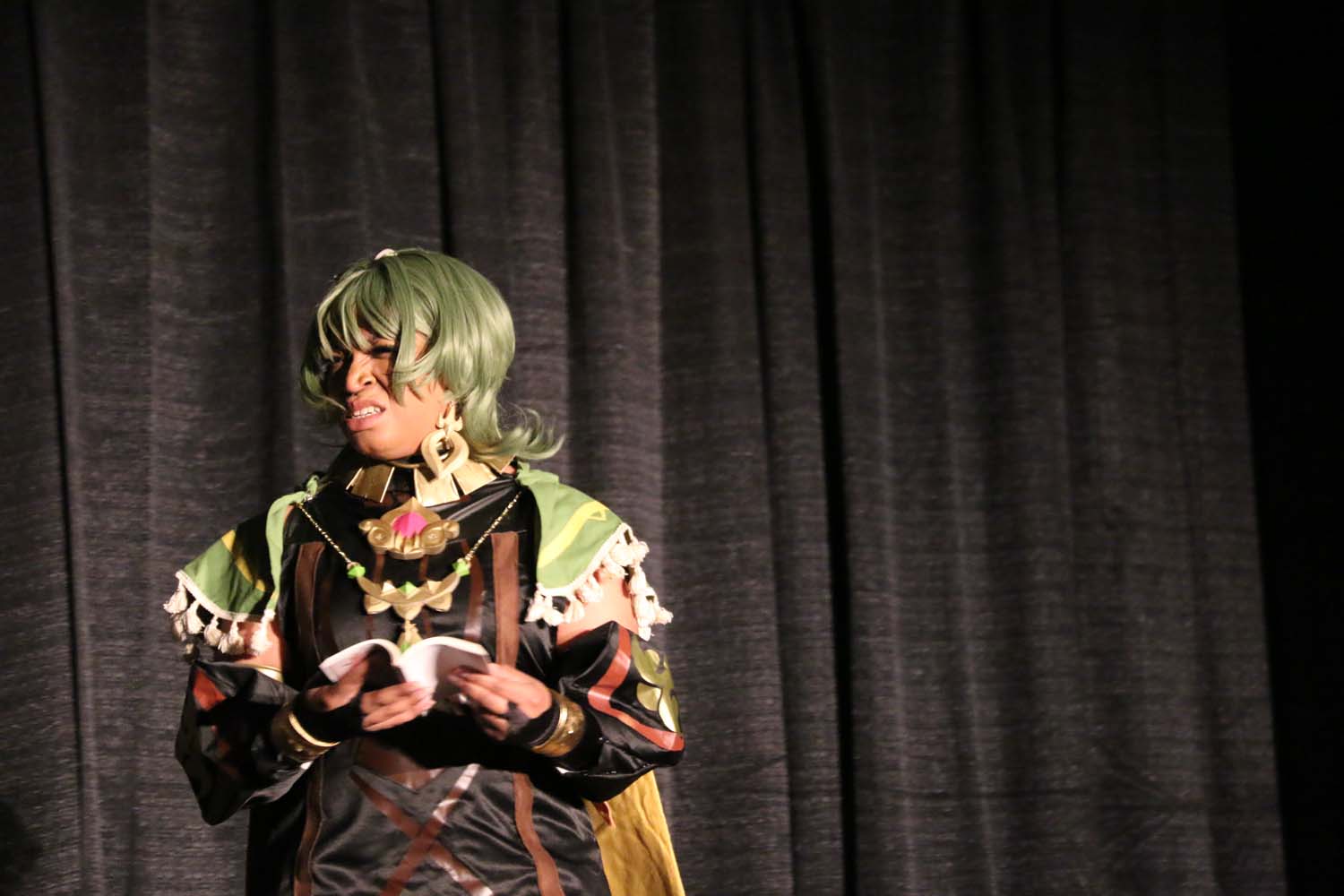
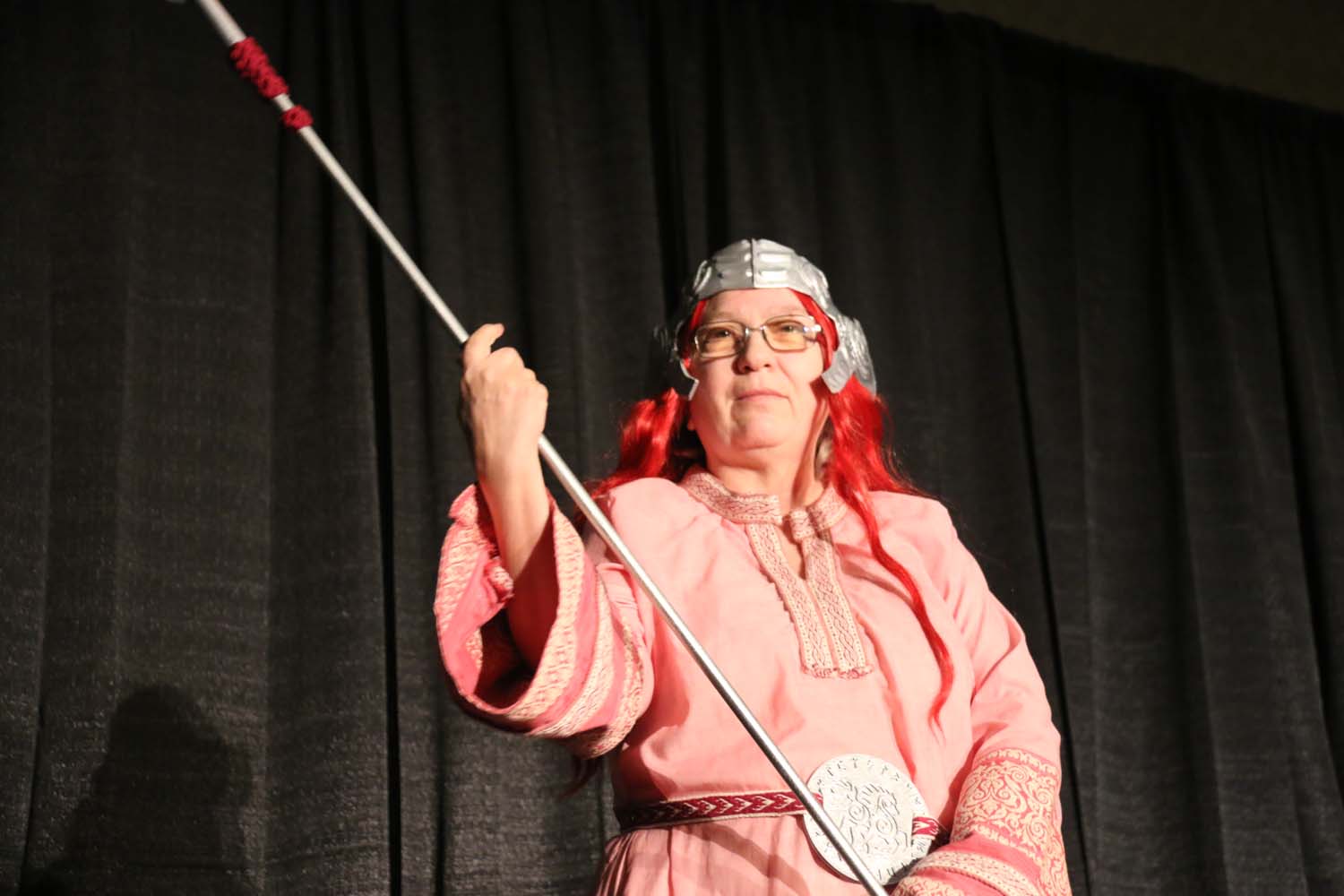
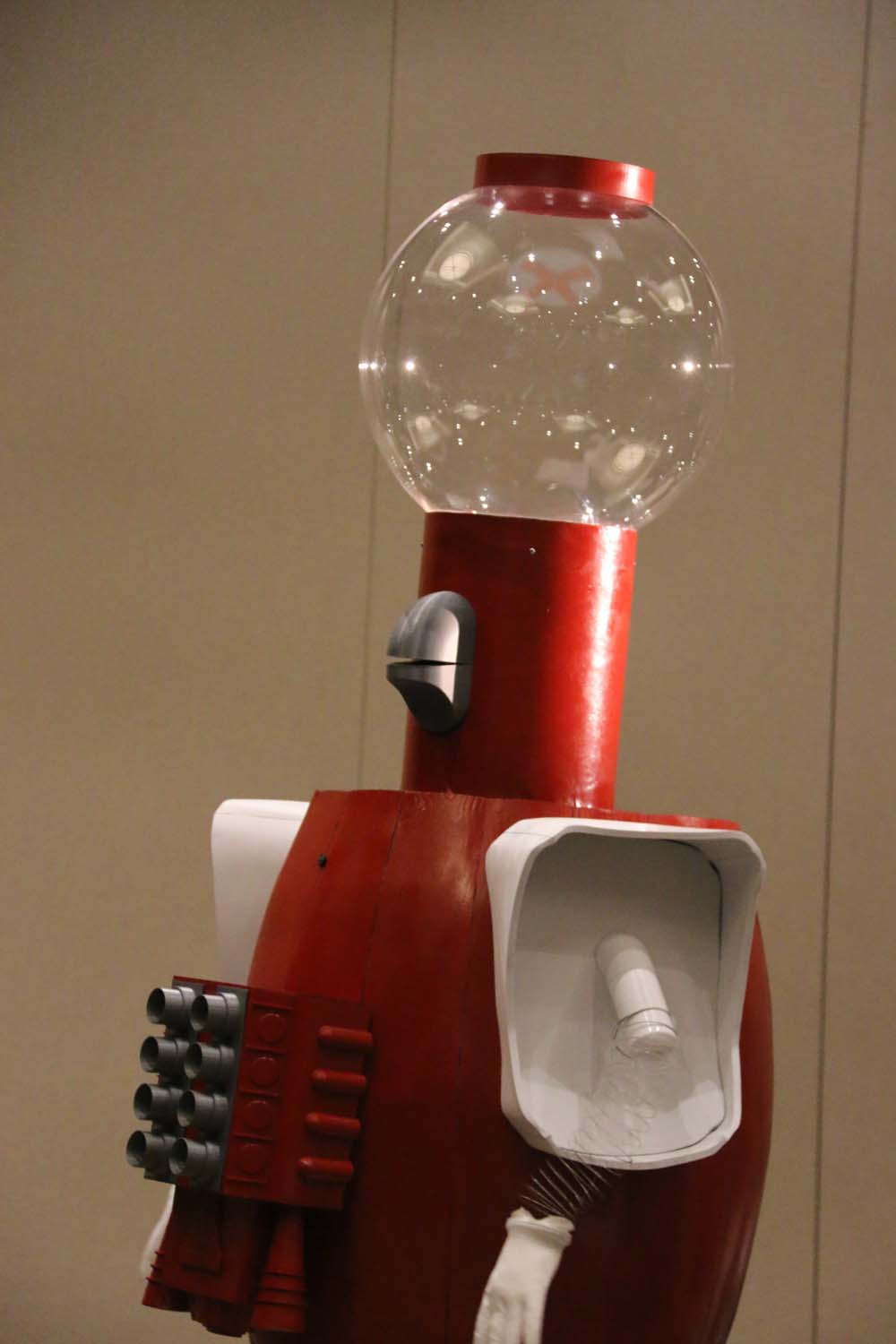
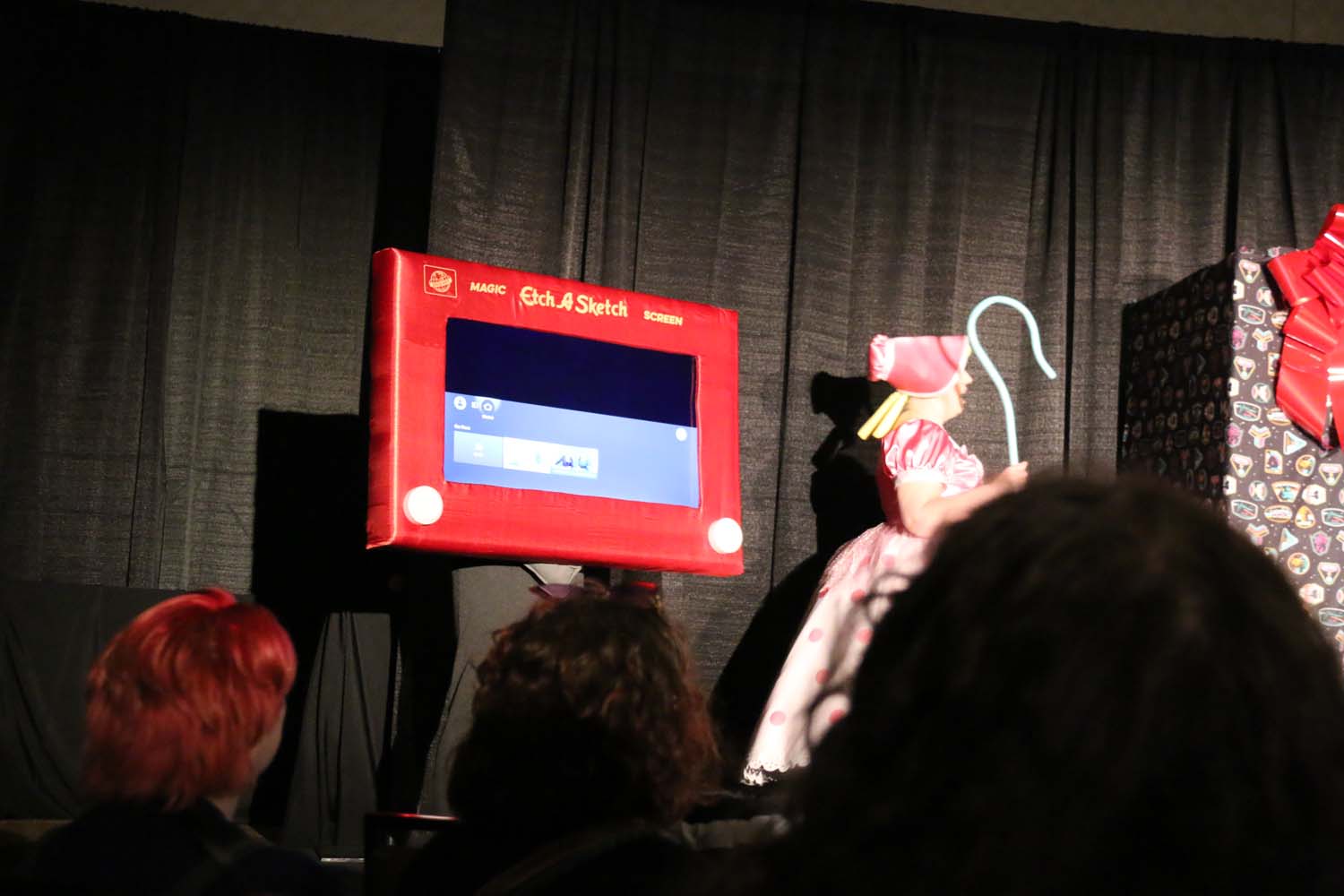
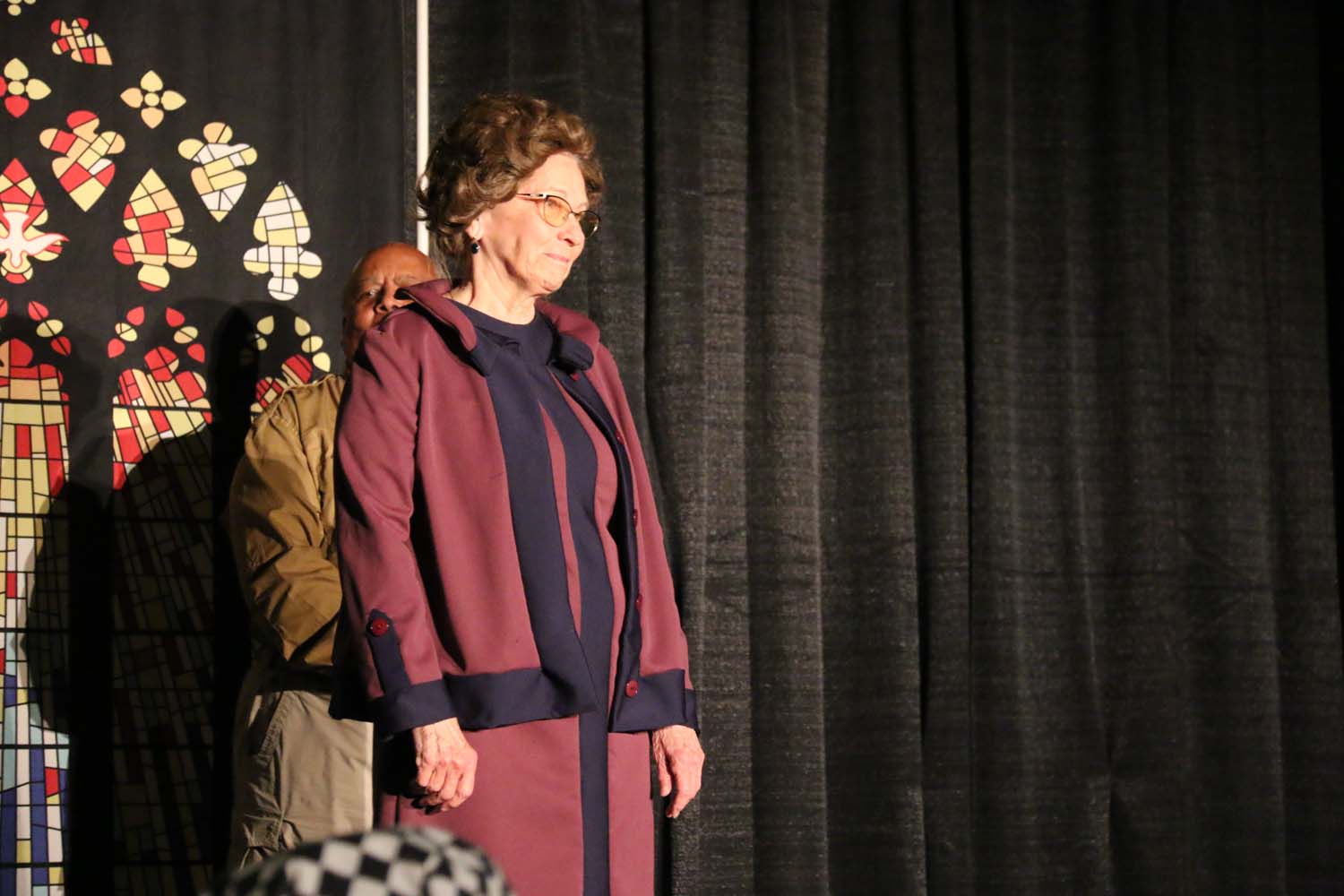
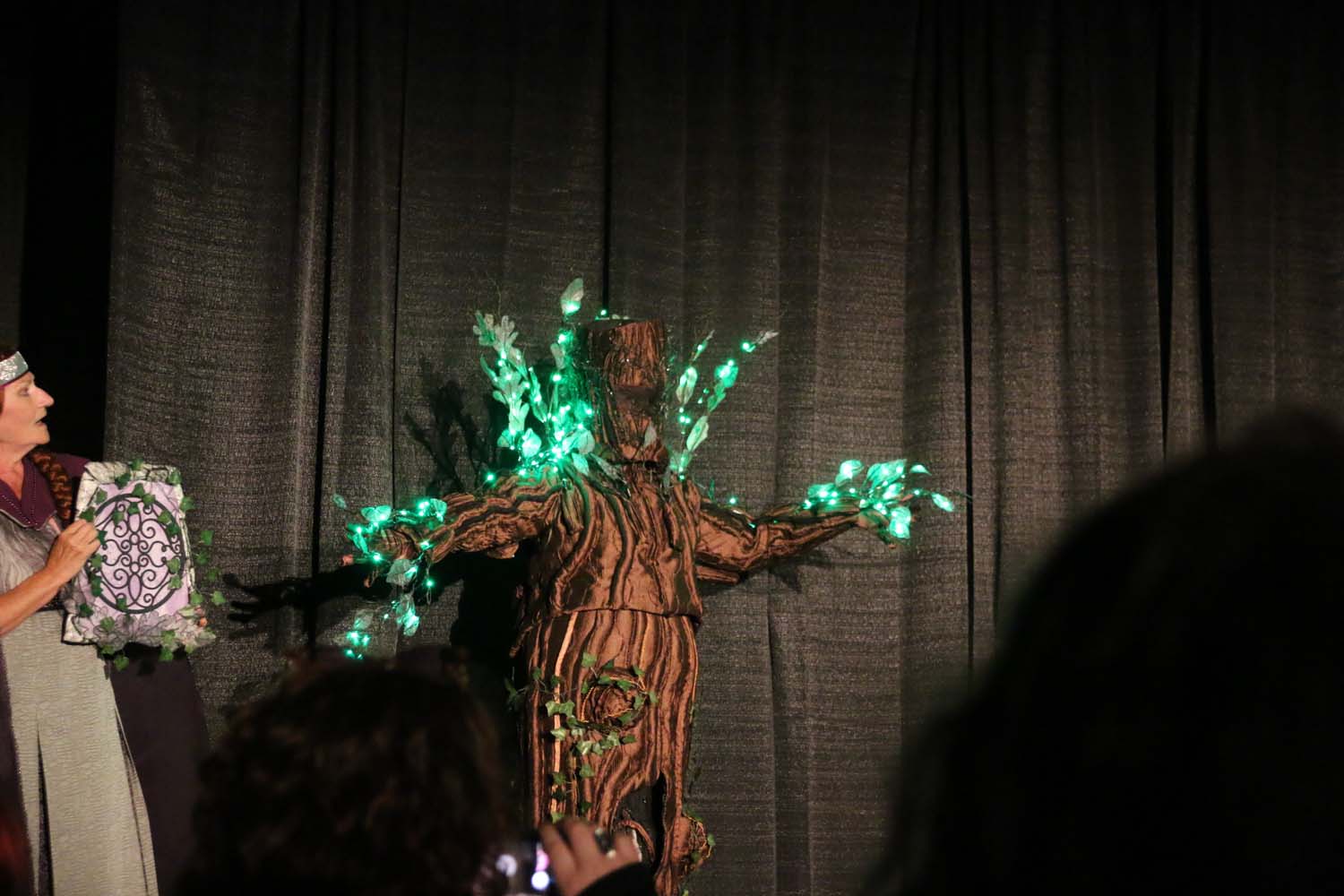
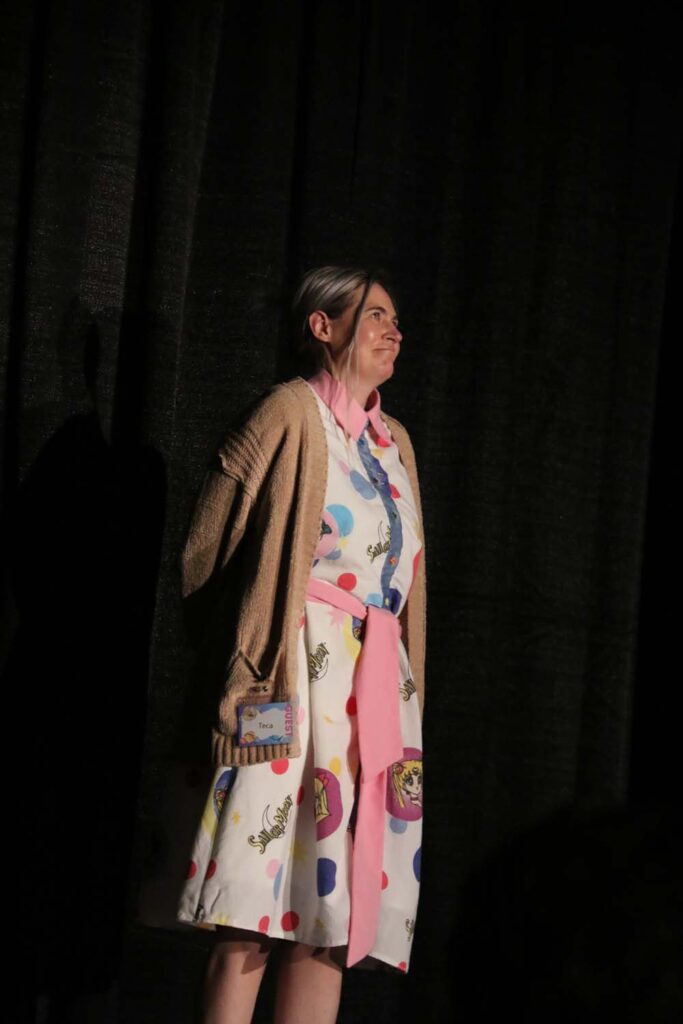
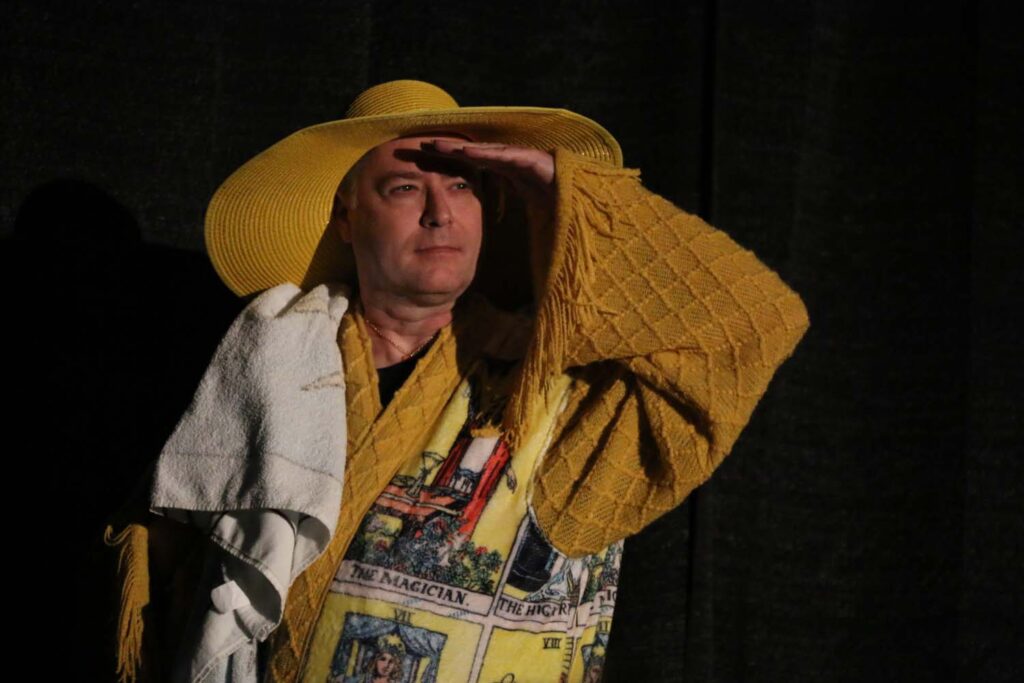
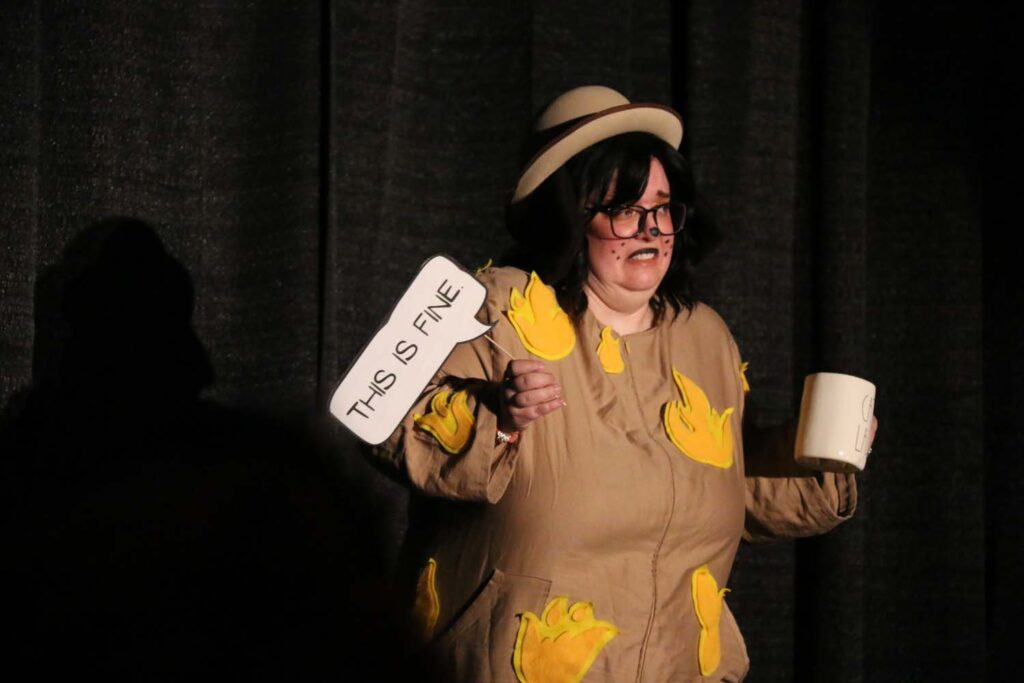
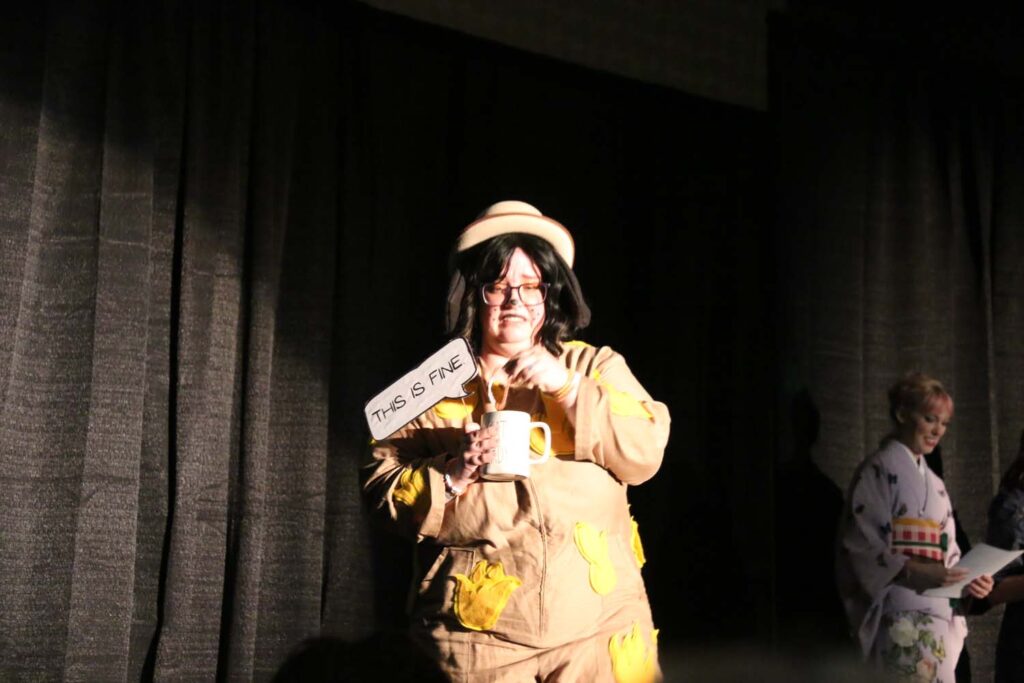
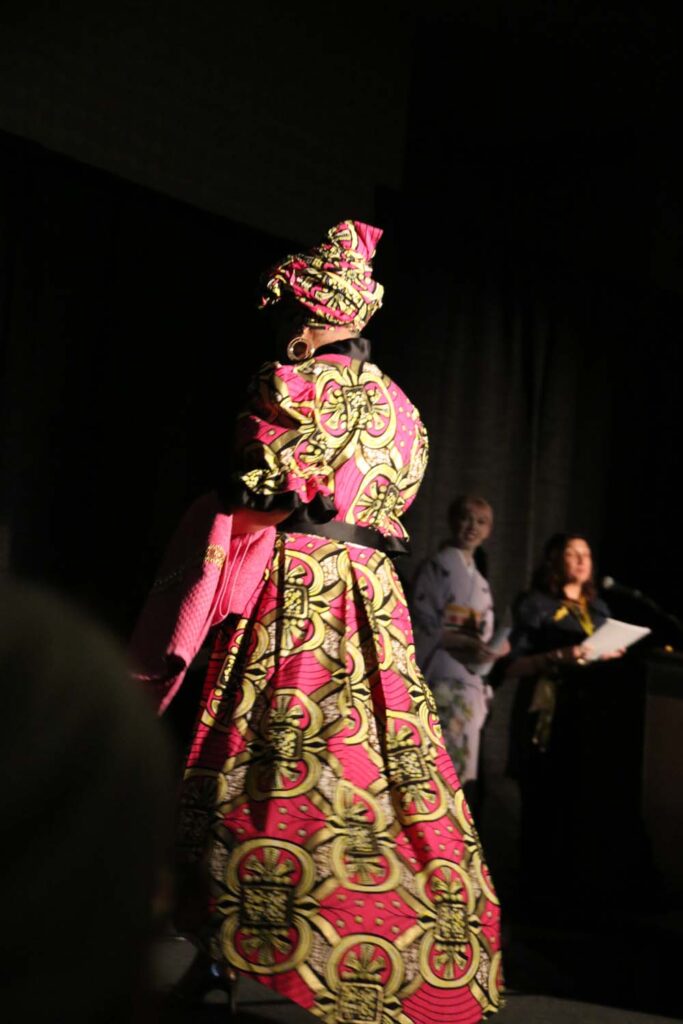
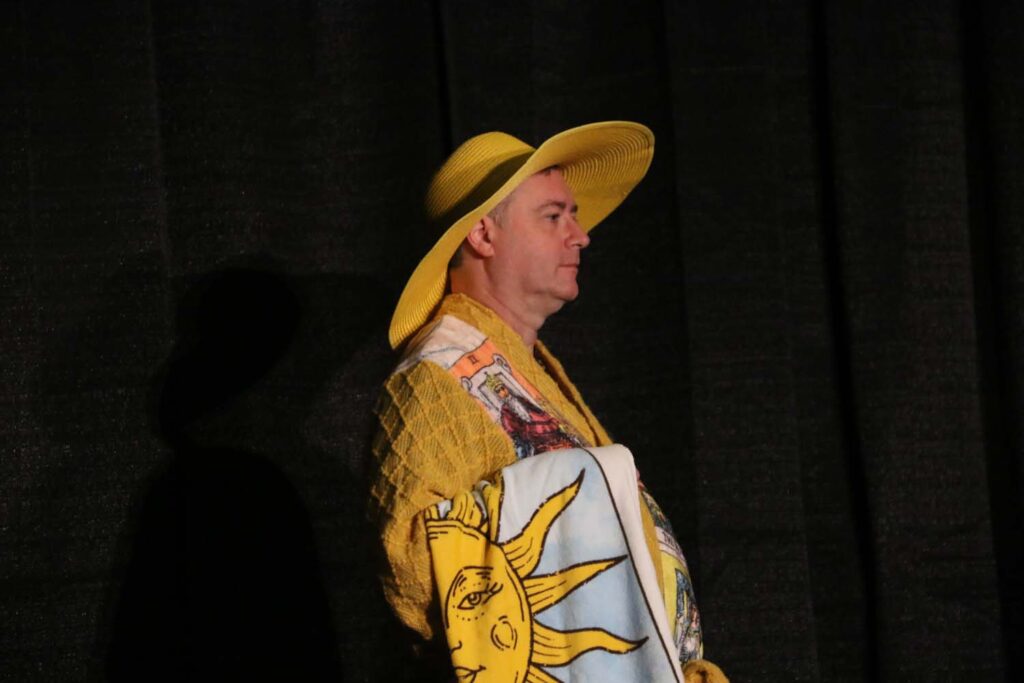
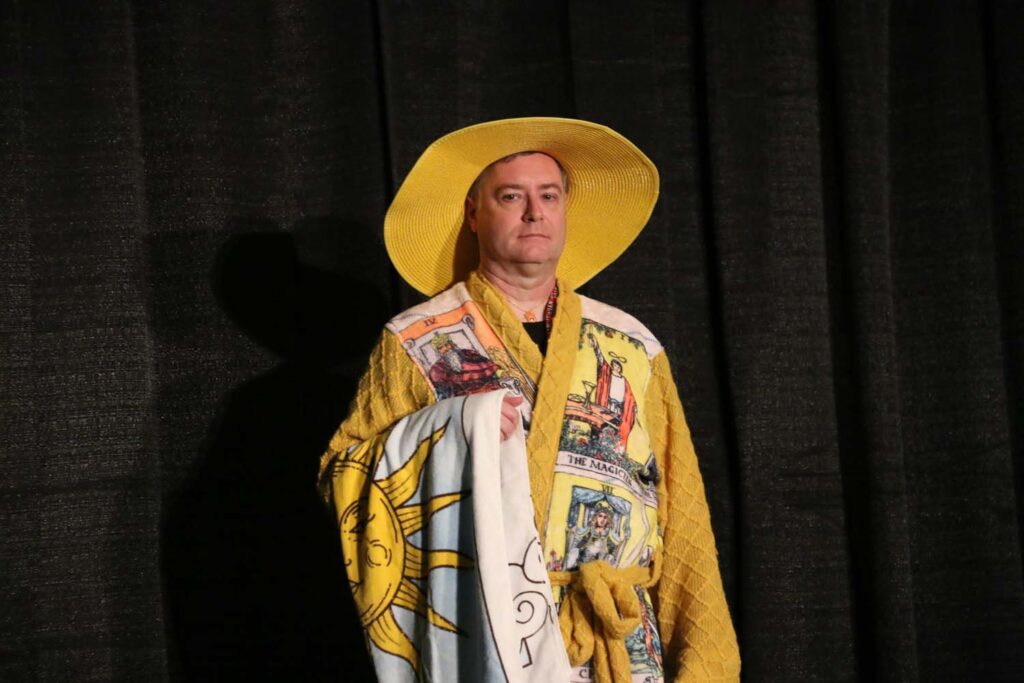
Costume-Con 42 – Saturday photos
Photos from the Science Fiction & Fantasy competition (both during the show and fan photography after). The photos are in no particular order.

























































































































































































































































Costume-Con 42 – Friday photos
Photos from the Single Pattern competition (both during the show and for fan photography after). The photos are not in any particular order.






































































Costume-Con 42
We attended Costume-Con 42 (CC42) over March 29 through April 1st, which was held in Aurora, Colorado. This was the successor to Costume-Con 39 which I co-chaired in 2023. The dates/numbers were scrambled with the pandemic, CC39 was held the year after CC40 (and took the place of CC41).
As with all Costume-Cons, the focus is on costuming in all of its varieties — SciFi, Historical, Anime, Cosplay, etc. The Friday night social is an opportunity to see old friends and make new ones, as well as see the Single Pattern Contest. The Single Pattern contest is a variety of people making their version of a specified pattern (usually one of 3-4), and showing it off to the crowd. This year’s patterns included a 3-piece suit, a bathrobe, and a jumpsuit. 17 folks showed off outfits made from one (or even two!) of these patterns.
Saturday focuses on SciFi and Fantasy, and 37 entries crossed the stage. The entries ranged from a 10 foot tall Tom Servo (from MST3K), to fairy princesses, to anime characters, you name it, it was there! Sunday focuses on the Historical costumes, with 13 entries ranging from the 2nd century to the 1960s.
There will be separate posts for each day, just because the number of photos is large. And the photos also include a variety of hall costuming.
Saturday Science Fiction & Fantasy photos
Sunday Historical photos
Hall Costume photos
References for the CSA 2024 Interesting Article Review
Afonso AM, Cadwell JB, Staffa SJ, Zurakowski D, Vinson AE. Burnout Rate and Risk Factors among Anesthesiologists in the United States. Anesthesiology [Internet]. 2021 May 1 [cited 2021 Aug 20];134(5):683–96. Available from: https://pubs.asahq.org/anesthesiology/article/134/5/683/115466/Burnout-Rate-and-Risk-Factors-among
Afonso AM, Cadwell JB, Staffa SJ, Sinskey, Vinson AE. U.S. Attending Anesthesiologist Burnout in the Postpandemic Era. Anesthesiology [Internet]. 2024 Jan [cited 2024 Mar 19];140(1):38–51. Available from: https://pubs.asahq.org/anesthesiology/article/140/1/38/139183/U-S-Attending-Anesthesiologist-Burnout-in-the?searchresult=1
Babcock L, Peyser B, Vesterlund L, Weingart L. Are You Taking on Too Many Non-Promotable Tasks? Harvard Business Review [Internet]. 2022 Apr 26 [cited 2023 Oct 25]; Available from: https://hbr.org/2022/04/are-you-taking-on-too-many-non-promotable-tasks
Bersoff DM, Sucher SJ, Tufano P. How Companies Should Weigh In on a Controversy. Harvard Business Review [Internet]. 2024 Mar 1 [cited 2024 Mar 17]; Available from: https://hbr.org/2024/03/how-companies-should-weigh-in-on-a-controversy
Bhakta NR, Bime C, Kaminsky DA, McCormack MC, Thakur N, Stanojevic S, et al. Race and Ethnicity in Pulmonary Function Test Interpretation: An Official American Thoracic Society Statement. Am J Respir Crit Care Med [Internet]. 2024 Apr 15 [cited 2024 Mar 19];207(8):978–95. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10112445/
Bline AP, DeWitt J c, Kwiatkowski CF, Pelch KE, Reade A, Varshavsky JR. Public Health Risks of PFAS-Related Immunotoxicity Are Real | Current Environmental Health Reports. Current Environmental Health Reports [Internet]. 2024 Mar 25 [cited 2024 Mar 28]; Available from: https://link.springer.com/article/10.1007/s40572-024-00441-y
Bonner SN, Lagisetty K, Reddy RM, Engeda Y, Griggs JJ, Valley TS. Clinical Implications of Removing Race-Corrected Pulmonary Function Tests for African American Patients Requiring Surgery for Lung Cancer. JAMA Surgery [Internet]. 2023 Oct 1 [cited 2024 Mar 23];158(10):1061–8. Available from: https://doi.org/10.1001/jamasurg.2023.3239
Burns NR, Kolarova T, Katz R, Ma K, Delaney S. Reconsidering Race Adjustment in Prenatal Alpha-Fetoprotein Screening. Obstetrics & Gynecology [Internet]. 2023 Mar [cited 2024 Mar 18];141(3):438. Available from: https://journals.lww.com/greenjournal/abstract/2023/03000/reconsidering_race_adjustment_in_prenatal.2.aspx
Crochemore T, Görlinger K, Lance MD. Early Goal-Directed Hemostatic Therapy for Severe Acute Bleeding Management in the Intensive Care Unit: A Narrative Review. Anesthesia & Analgesia [Internet]. 2024 Mar [cited 2024 Mar 7];138(3):499. Available from: https://journals.lww.com/anesthesia-analgesia/fulltext/2024/03000/early_goal_directed_hemostatic_therapy_for_severe.6.aspx
Ehsan MN, Riza M, Pervez MdN, Khyum MMO, Liang Y, Naddeo V. Environmental and health impacts of PFAS: Sources, distribution and sustainable management in North Carolina (USA). Science of The Total Environment [Internet]. 2023 Jun 20 [cited 2024 Mar 28];878:163123. Available from: https://www.sciencedirect.com/science/article/pii/S0048969723017424
Etherington C, Boet S, Chen I, Duffy M, Mamas MA, Eddeen AB, et al. Association between Surgeon/anesthesiologist Sex Discordance and One-year Mortality Among Adults Undergoing Noncardiac Surgery: A Population-based Retrospective Cohort Study. Annals of Surgery [Internet]. 2024 Apr [cited 2024 Feb 14];10.1097/SLA.0000000000006111. Available from: https://journals.lww.com/annalsofsurgery/abstract/9900/association_between_surgeon_anesthesiologist_sex.658.aspx
Fleisher LA, Lane-Fall M. Surgery as a Team Sport: Can Team Composition Influence Patient Outcomes? Annals of Surgery [Internet]. 2024 Apr [cited 2024 Mar 19];279(4):575–6. Available from: https://journals.lww.com/10.1097/SLA.0000000000006206
Gallos I, Devall A, Martin J, Middleton L, Beeson L, Galadanci H, et al. Randomized Trial of Early Detection and Treatment of Postpartum Hemorrhage. New England Journal of Medicine [Internet]. 2023 Jul 6 [cited 2024 Mar 8];389(1):11–21. Available from: https://doi.org/10.1056/NEJMoa2303966
Hughes ZH, Hughes LM, Huang X, Petito LC, Grobman WA, Khan SS. Changes in Age Distribution and Maternal Mortality in a Subset of the US, 2014–2021. American Journal of Preventive Medicine [Internet]. 2024 Mar 18 [cited 2024 Mar 27]; Available from: https://www.sciencedirect.com/science/article/pii/S0749379724000655
Jerath A, Satkunasivam R, Kaneshwaran K, Aminoltejari K, Chang A, MacDonell DSY, et al. Association Between Anesthesiologist Sex and Patients’ Postoperative Outcomes: A Population-based Cohort Study. Annals of Surgery [Internet]. 2024 Apr [cited 2024 Feb 11];10.1097/SLA.0000000000006217. Available from: https://journals.lww.com/annalsofsurgery/pages/articleviewer.aspx?year=9900&issue=00000&article=00759&type=Abstract
Joseph KS, Lisonkova S, Boutin A, Muraca GM, Razaz N, John S, et al. Maternal mortality in the United States: are the high and rising rates due to changes in obstetrical factors, maternal medical conditions, or maternal mortality surveillance? American Journal of Obstetrics & Gynecology [Internet]. 2024 Mar 12 [cited 2024 Mar 17];0(0). Available from: https://www.ajog.org/article/S0002-9378(24)00005-X/fulltext
Marfella R, Prattichizzo F, Sardu C, Fulgenzi G, Graciotti L, Spadoni T, et al. Microplastics and Nanoplastics in Atheromas and Cardiovascular Events. New England Journal of Medicine [Internet]. 2024 Mar 7 [cited 2024 Mar 8];390(10):900–10. Available from: https://doi.org/10.1056/NEJMoa2309822
Mathis MR, Schonberger RB, Whitlock EL, Vogt KM, Lagorio JE, Jones KA, et al. Opportunities Beyond the Anesthesiology Department: Broader Impact Through Broader Thinking. Anesthesia & Analgesia [Internet]. 2022 Feb [cited 2024 Mar 4];134(2):242. Available from: https://journals.lww.com/anesthesia-analgesia/fulltext/2022/02000/opportunities_beyond_the_anesthesiology.5.aspx
Mondal S, Oakes D, Humphrey T, Kolarczyk L, Trzcinka A. Women in Anesthesiology and the Mid-Career Stall: Why They Are Not Advancing Into Senior Leadership. Anesthesia & Analgesia [Internet]. 2024 Jan 30 [cited 2024 Mar 22];10.1213/ANE.0000000000006826. Available from: https://journals.lww.com/anesthesia-analgesia/abstract/9900/women_in_anesthesiology_and_the_mid_career_stall_.716.aspx
Sen S, Potnuru PP, Hernandez N, Goehl C, Praestholm C, Sridhar S, et al. Glucagon-Like Peptide-1 Receptor Agonist Use and Residual Gastric Content Before Anesthesia. JAMA Surgery [Internet]. 2024 Mar 6 [cited 2024 Mar 17]; Available from: https://doi.org/10.1001/jamasurg.2024.0111
Wallis CJD, Jerath A, Aminoltejari K, Kaneshwaran K, Salles A, Coburn N, et al. Surgeon Sex and Long-Term Postoperative Outcomes Among Patients Undergoing Common Surgeries. JAMA Surgery [Internet]. 2023 Aug 30 [cited 2023 Aug 31]; Available from: https://doi.org/10.1001/jamasurg.2023.3744
Wallis CJD, Jerath A, Kaneshwaran K, Hallet J, Coburn N, Wright FC, et al. Association Between Surgeon and Anesthesiologist Sex Discordance and Postoperative Outcomes: A Population-based Cohort Study. Annals of Surgery [Internet]. 2022 Jul [cited 2024 Feb 13];276(1):81–7. Available from: https://journals.lww.com/10.1097/SLA.0000000000005495
Yeo YH, Gaddam S, Ng WH, Huang PC, Mohamed G, Samaan J, et al. Increased risk of aspiration pneumonia associated with endoscopic procedures among patients with Glucagon-like peptide-1 receptor agonist use. Gastroenterology [Internet]. 2024 Mar 27 [cited 2024 Mar 29];0(0). Available from: https://www.gastrojournal.org/article/S0016-5085(24)00298-1/abstract?fbclid=IwAR1_hsWNkE_s5x7EB8cEinuhh4K-q0elPoxQE077NWrDCeXlfIk6OVWx5js_aem_ActnmV586uZM-nUzWLoSdofydnokWRGOKvRIzWEF3dD65weGSbE2sWlMSBuBMl9gYs2ESzaF7btISB6oYcCkegh_
Zhu L, Zhu J, Zuo R, Xu Q, Qian Y, An L. Identification of microplastics in human placenta using laser direct infrared spectroscopy. Science of The Total Environment [Internet]. 2023 Jan 15 [cited 2024 Mar 29];856:159060. Available from: https://www.sciencedirect.com/science/article/pii/S0048969722061599
Joel Bervell [Internet]. [cited 2024 Mar 30]. Available from: https://joelbervell.com/#homepage
References for Human Factors in Healthcare
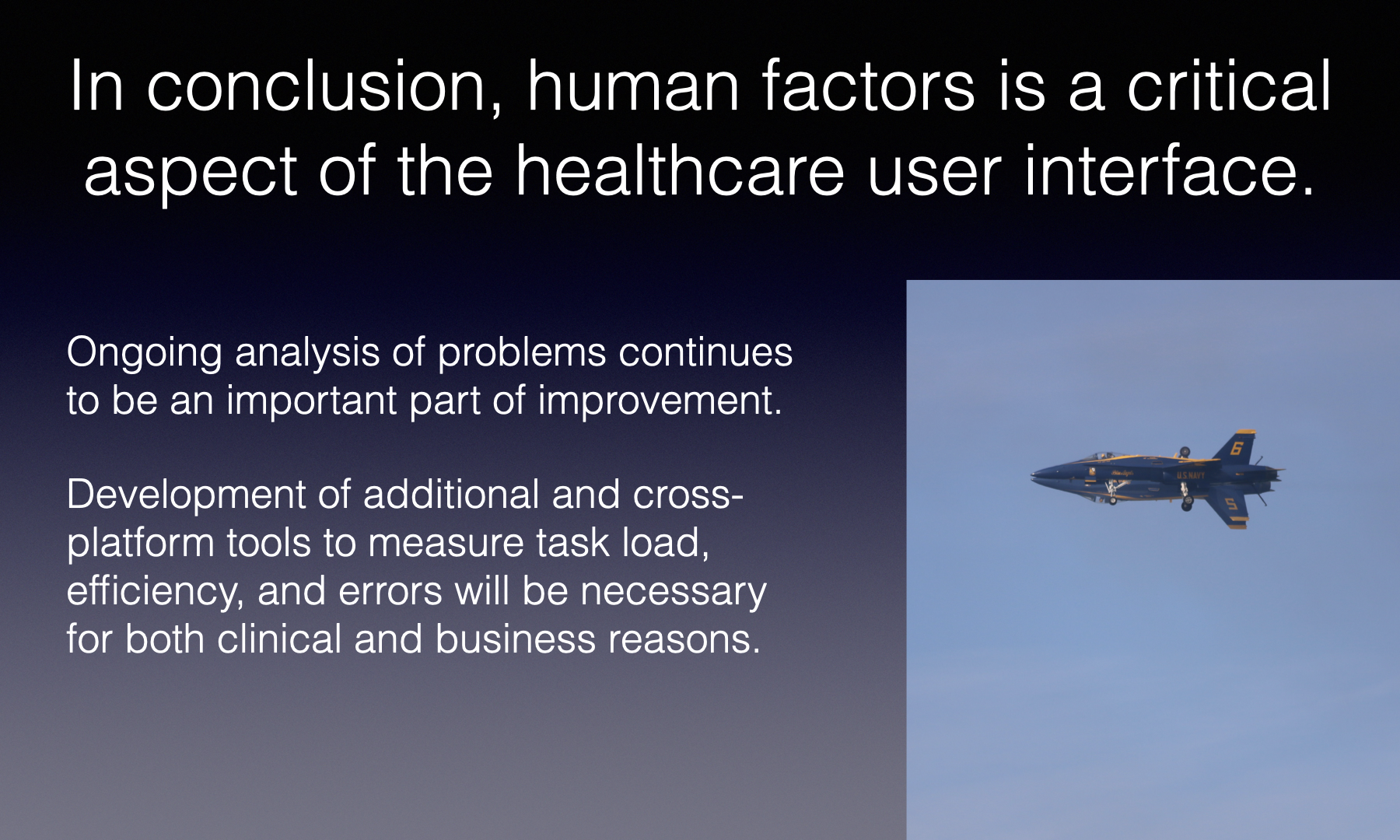
These references are for the presentation “The Importance of Human Factors in Healthcare User Interfaces” which was created as part of the OHSU course on scientific writing (BMI 570).
Safety and effectiveness of health IT software and systems—Part 4: Application of human factors engineering. AAMI HIT1000-4 (PS):2020; Safety and effectiveness of health IT software and systems—Part 4: Application of human factors engineering . 2020
Ahmed A, Chandra S, Herasevich V, Gajic O, Pickering BW. The effect of two different electronic health record user interfaces on intensive care provider task load, errors of cognition, and performance. Crit Care Med. 2011 Jul;39(7):1626–34.
AQI – Anesthesia Incident Reporting System [Internet]. [cited 2023 Dec 2]. Available from: https://www.aqihq.org/airsIntro.aspx
ASRS – Aviation Safety Reporting System [Internet]. [cited 2023 Nov 25]. Available from: https://asrs.arc.nasa.gov/
Bakken S. Hot topics in clinical informatics. J Am Med Inform Assoc. 2020 Mar 16;27(4):503–4.
Bannister B. freeCodeCamp.org. 2017 [cited 2023 Oct 26]. Why typography matters — Especially at the Oscars. Available from: https://www.freecodecamp.org/news/why-typography-matters-especially-at-the-oscars-f7b00e202f22/
Barkman RC. Why the human brain is so good at detecting patterns | Psychology Today [Internet]. [cited 2023 Oct 27]. Available from: https://www.psychologytoday.com/us/blog/singular-perspective/202105/why-the-human-brain-is-so-good-detecting-patterns
Berry JM, Loeb RG. 18 – Ergonomics of the Anesthesia Workspace. In: Ehrenwerth J, Eisenkraft JB, Berry JM, editors. Anesthesia Equipment (Third Edition) [Internet]. Philadelphia: W.B. Saunders; 2021 [cited 2023 Dec 1]. p. 407–30. Available from: https://www.sciencedirect.com/science/article/pii/B9780323672795000182
Classen DC, Longhurst CA, Davis T, Milstein JA, Bates DW. Inpatient EHR user experience and hospital EHR safety performance. JAMA Network Open. 2023 Sep 11;6(9):e2333152.
D’Souza C, Paquet V, Steinfeld E. Clearance space envelopes of wheeled mobility device users for computer workstations. Proceedings of the Human Factors and Ergonomics Society Annual Meeting. 2012 Sep 1;56(1):2373–7.
de Ridder D, de Ridder J, Reinders MJT. Pattern recognition in bioinformatics. Briefings in Bioinformatics. 2013 Sep 1;14(5):633–47.
Diehl C, Martins A, Almeida A, Silva T, Ribeiro Ó, Santinha G, et al. Defining recommendations to guide user interface design: Multimethod approach. JMIR Hum Factors. 2022 Sep 30;9(3):e37894.
Federal Aviation Administration. AC25.1322.1 FAA Advisory Circular: Flightcrew Alerting. Washington, D.C.; 2010.
Fleming JW. Washington Post. 2023 [cited 2023 Nov 12]. Opinion | Countless kids are colorblind — and don’t know about it. Here’s how to help. Available from: https://www.washingtonpost.com/opinions/2023/11/07/colorblind-children-testing-school/
Gause DC, Weinberg GM. Exploring requirements: quality before design. New York, NY: Dorset House Pub.; 1989.
Gellert GA, Crouch JF, Gibson LA, Conklin GS, Webster SL, Gillean JA. Clinical impact and value of workstation single sign-on. International Journal of Medical Informatics. 2017 May 1;101:131–6.
Grailey K, Leon-Villapalos C, Murray E, Brett SJ. The psychological impact of the workplace environment in critical care: A qualitative exploration. Human Factors in Healthcare. 2021 Dec 1;1:100001.
HFES | Human Factors and Ergonomics Society [Internet]. [cited 2023 Oct 5]. Available from: https://www.hfes.org/
HFES. ANSI/HFES 100-2007 – Human Factors Engineering of Computer Workstations. Santa Monica, CA; 2007. [cited 2023 Nov 22]. Available from: https://webstore.ansi.org/standards/hfes/ansihfes1002007
HFES. ANSI/HFES 200-2008 – Human Factors Engineering of Software User Interfaces [Internet]. 2008 [cited 2023 Oct 18]. Available from: https://webstore.ansi.org/standards/hfes/ansihfes2002008
Hron JD, Lourie E. Have you got the time? Challenges using vendor electronic health record metrics of provider efficiency. Journal of the American Medical Informatics Association. 2020 Apr 1;27(4):644–6.
Health and Safety Executive [Internet]. [cited 2023 Nov 1]. HSE: Information about health and safety at work. Available from: https://www.hse.gov.uk/
HSE. Display screen equipment (DSE) workstation checklist [Internet]. [cited 2023 Nov 11]. Available from: hse.gov.uk/pubns/ck1.htm
Leviss J, editor. HIT or Miss: Lessons Learned From Health Information Technology Projects. Third edition. Boca Raton London New York: CRC Press; 2019. 246 p.
McKee C, Hedge A. Ergonomic lighting considerations for the home office workplace. Davis K, Kotowski S, editors. WOR. 2022 Feb 18;71(2):335–43.
Merchant RM, Topjian AA, Panchal AR, Cheng A, Aziz K, Berg KM, et al. Part 1: Executive summary: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020 Oct 20;142(16_suppl_2):S337–57.
Moran K. Nielsen Norman Group. 2019 [cited 2023 Nov 11]. Usability Testing 101. Available from: https://www.nngroup.com/articles/usability-testing-101/
TLX @ NASA Ames – Home [Internet]. [cited 2023 Nov 11]. Available from: https://humansystems.arc.nasa.gov/groups/tlx/
Nelson O, Greenwood E, Simpao AF, Matava CT. Refocusing on work-based hazards for the anaesthesiologist in a post-pandemic era. BJA Open [Internet]. 2023 Dec 1 [cited 2023 Nov 1];8. Available from: https://www.bjaopen.org/article/S2772-6096(23)00113-2/fulltext
Nielsen J. Nielsen Norman Group. [cited 2023 Nov 24]. Usability 101: Introduction to usability. Available from: https://www.nngroup.com/articles/usability-101-introduction-to-usability/
NIOSH – Anthropometry https://www.cdc.gov/niosh/topics/anthropometry/default.html
Norman DA. The design of everyday things. Revised and expanded edition. New York, New York: Basic Books; 2013. 347 p.
Reid CR, Johnson PW, Marklin RW, Seeley P, Spielholz P, Goggins R. Communicating the value of ergonomics to management – Part 2: Ergonomics ROI case study applications. Proceedings of the Human Factors and Ergonomics Society Annual Meeting. 2017 Sep 1;61(1):973–5.
Rempel D, Reid CR, McGowan B, Williamson C, Alexander D, Whitehead C, et al. Communicating the value of ergonomics to management – Part 1: Language, ROI, and models. Proceedings of the Human Factors and Ergonomics Society Annual Meeting. 2017 Sep 1;61(1):920–3.
Rosenholtz R, Li Y, Nakano L. Measuring visual clutter. Journal of Vision. 2007 Aug 16;7(2):17.
Ruskin KJ, Corvin C, Rice S, Richards G, Winter SR, Clebone Ruskin A. Alarms, alerts, and warnings in air traffic control: An analysis of reports from the Aviation Safety Reporting System. Transportation Research Interdisciplinary Perspectives. 2021 Dec 1;12:100502.
Saitwal H, Feng X, Walji M, Patel V, Zhang J. Assessing performance of an electronic health record (EHR) using cognitive task analysis. International Journal of Medical Informatics. 2010 Jul 1;79(7):501–6.
Shanafelt TD, Larson D, Bohman B, Roberts R, Trockel M, Weinlander E, et al. Organization-wide approaches to foster effective unit-level efforts to improve clinician well-being. Mayo Clinic Proceedings. 2023 Jan 1;98(1):163–80.
Shugen W. Framework of pattern recognition model based on the cognitive psychology. Geo-spatial Information Science. 2002 Jan 1;5(2):74–8.
Sinsky CA, Rule A, Cohen G, Arndt BG, Shanafelt TD, Sharp CD, et al. Metrics for assessing physician activity using electronic health record log data. Journal of the American Medical Informatics Association. 2020 Apr 1;27(4):639–43.
Stanford Medicine. Doctors call for overhaul of electronic health records [Internet]. [cited 2023 Oct 11]. Available from: https://www.prnewswire.com/news-releases/doctors-call-for-overhaul-of-electronic-health-records-300659100.html
Tang PC, Patel VL. Major issues in user interface design for health professional workstations: summary and recommendations. Int J Biomed Comput. 1994 Jan;34(1–4):139–48.
Tracy D. The Autopian. 2022 [cited 2023 Oct 28]. Here’s the official reason why some traffic lights are horizontal and some are vertical. Available from: https://www.theautopian.com/heres-the-official-reason-why-some-traffic-lights-are-horizontal-and-some-are-vertical/
Wachter RM. The digital doctor: hope, hype, and harm at the dawn of medicine’s computer age. New York: McGraw-Hill Education; 2017. 330 p. (Business classics).
References for Post-COVID presentation
This reference list was created for the presentation “Post-COVID: What do we need to know?”
It was updated March 2023
A clinical case definition of post COVID-19 condition by a Delphi consensus, 6 October 2021 [Internet]. [cited 2022 Oct 31]. Available from: https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1
Abraham S, Nohria A, Neilan TG, Asnani A, Saji AM, Shah J, et al. Cardiovascular Drug Interactions With Nirmatrelvir/Ritonavir in Patients With COVID-19: JACC Review Topic of the Week. Journal of the American College of Cardiology [Internet]. 2022 Jul 21 [cited 2022 Oct 15]; Available from: https://www.jacc.org/doi/10.1016/j.jacc.2022.08.800
ACOG. COVID-19, Pregnancy, Childbirth, and Breastfeeding: Answers From Ob-Gyns [Internet]. [cited 2022 Nov 10]. Available from: https://www.acog.org/en/womens-health/faqs/coronavirus-covid-19-pregnancy-and-breastfeeding
American Society of Anesthesiologists, Anesthesia Patient Safety Foundation. ASA and APSF Joint Statement on Elective Surgery and Anesthesia for Patients after COVID-19 Infection [Internet]. 2021 [cited 2022 Nov 6]. Available from: https://www.asahq.org/about-asa/newsroom/news-releases/2021/03/asa-and-apsf-joint-statement-on-elective-surgery-and-anesthesia-for-patients-after-covid-19-infection-rv
Andersen KM, Bates BA, Rashidi ES, Olex AL, Mannon RB, Patel RC, et al. Long-term use of immunosuppressive medicines and in-hospital COVID-19 outcomes: a retrospective cohort study using data from the National COVID Cohort Collaborative. The Lancet Rheumatology. 2022 Jan 1;4(1):e33–41. https://doi.org/10.1016/S2665-9913(21)00325-8
Bleumink GS, Knetsch AM, Sturkenboom MCJM, Straus SMJM, Hofman A, Deckers JW, et al. Quantifying the heart failure epidemic: prevalence, incidence rate, lifetime risk and prognosis of heart failure: The Rotterdam Study. European Heart Journal. 2004 Sep 1;25(18):1614–9. https://doi.org/10.1016/j.ehj.2004.06.038
Bowe B, Xie Y, Al-Aly Z. Acute and postacute sequelae associated with SARS-CoV-2 reinfection. Nat Med. 2022 Nov 10;1–8.
https://doi.org/10.1038/s41591-022-02051-3
Cambou, MC, et al. Longitudinal Evaluation of Antibody Persistence in Mother-Infant Dyads After Severe Acute Respiratory Syndrome Coronavirus 2 Infection in Pregnancy | The Journal of Infectious Diseases | Oxford Academic [Internet]. [cited 2022 Oct 14]. Available from: https://academic.oup.com/jid/advance-article/doi/10.1093/infdis/jiac366/6694708?searchresult=1&login=false
Cha AE. How covid brain fog may overlap with ‘chemo brain’ and Alzheimer’s. Washington Post [Internet]. 2022 Mar 27 [cited 2022 Mar 28]; Available from: https://www.washingtonpost.com/health/2022/03/27/covid-brain-fog-chemo-brain-alzheimers-disease/
CMS. New COVID-19 Treatments Add-On Payment (NCTAP) [Internet]. CMS.gov. [cited 2022 Nov 8]. Available from: https://www.cms.gov/medicare/covid-19/new-covid-19-treatments-add-payment-nctap
Deng JZ, Chan JS, Potter AL, Chen YW, Sandhu HS, Panda N, et al. The Risk of Postoperative Complications following Major Elective Surgery in Active or Resolved COVID-19 in the United States. Annals of Surgery. 2022 Feb;275(2):242–6.
Dickson A. Opera Singers Help Covid-19 Patients Learn to Breathe Again. The New York Times [Internet]. 2021 Feb 16 [cited 2022 Nov 6]; Available from: https://www.nytimes.com/2021/02/16/arts/music/opera-singers-covid-19-treatment-eno-breathe.html
Fernández-Castañeda A, Lu P, Geraghty AC, Song E, Lee MH, Wood J, et al. Mild respiratory COVID can cause multi-lineage neural cell and myelin dysregulation. Cell. 2022 Jul 7;185(14):2452-2468.e16. https://dx.doi.org/10.1016/j.cell.2022.06.008
Frésard I, Genecand L, Altarelli M, Gex G, Vremaroiu P, Vremaroiu-Coman A, et al. Dysfunctional breathing diagnosed by cardiopulmonary exercise testing in ‘long COVID’ patients with persistent dyspnoea. BMJ Open Respiratory Research. 2022 Mar 1;9(1):e001126. https://doi.org/10.1136/bmjresp-2021-001126
Global Burden of Disease Long COVID Collaborators. Estimated Global Proportions of Individuals With Persistent Fatigue, Cognitive, and Respiratory Symptom Clusters Following Symptomatic COVID-19 in 2020 and 2021. JAMA [Internet]. 2022 Oct 10 [cited 2022 Oct 20]; Available from: https://doi.org/10.1001/jama.2022.18931
Gray L. Long COVID: Learning as We Go [Internet]. [cited 2022 Nov 2]. Available from: https://www.idse.net/Covid-19/Article/06-22/Long-COVID-Learning-as-We-Go/67080?ses=ogst
Hastie CE, Lowe DJ, McAuley A, Winter AJ, Mills NL, Black C, et al. Outcomes among confirmed cases and a matched comparison group in the Long-COVID in Scotland study. Nat Commun. 2022 Oct 12;13(1):5663. https://doi.org/10.1038/s41467-022-33415-5
Huang L, Li X, Gu X, Zhang H, Ren L, Guo L, et al. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: a longitudinal cohort study. The Lancet Respiratory Medicine [Internet]. 2022 May 11 [cited 2022 May 22];0(0). Available from: https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(22)00126-6/fulltext
Hunni Media. Covid and the brain: A neurological health crisis. Knowable Magazine [Internet]. 2022 May 25 [cited 2022 Nov 9]; Available from: https://knowablemagazine.org/article/health-disease/2022/covid-and-brain-neurological-health-crisis
Klein SL. Sex influences immune responses to viruses, and efficacy of prophylaxis and treatments for viral diseases. BioEssays. 2012;34(12):1050–9. https://onlinelibrary.wiley.com/doi/abs/10.1002/bies.201200099
Knight R, Walker V, Ip S, Cooper JA, Bolton T, Keene S, et al. Association of COVID-19 With Major Arterial and Venous Thrombotic Diseases: A Population-Wide Cohort Study of 48 Million Adults in England and Wales. Circulation. 2022 Sep 20;146(12):892–906. https://doi.org/10.1161/CIRCULATIONAHA.122.060785
McCreary EK, Lemon L, Megli C, Oakes A, Seymour CW. Monoclonal Antibodies for Treatment of SARS-CoV-2 Infection During Pregnancy. Ann Intern Med [Internet]. 2022 Nov 15 [cited 2022 Nov 15]; Available from: https://www.acpjournals.org/doi/10.7326/M22-1329
Merad M, Blish CA, Sallusto F, Iwasaki A. The immunology and immunopathology of COVID-19. Science. 2022 Mar 11;375(6585):1122–7. https://doi.org/10.1126/science.abm8108
Metz TD, Clifton RG, Hughes BL, Sandoval GJ, Grobman WA, Saade GR, et al. Association of SARS-CoV-2 Infection With Serious Maternal Morbidity and Mortality From Obstetric Complications. JAMA. 2022 Feb 22;327(8):748–59. https://doi.org/10.1001/jama.2022.1190
Nepogodiev D, Bhangu A, Glasbey JC, Li E, Omar OM, Simoes JF, et al. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. The Lancet. 2020 Jul 4;396(10243):27–38. https://doi.org/10.1016/S0140-6736(20)31182-X
NIH. Anti-SARS-CoV-2 Antibody Products Summary Recommendations [Internet]. COVID-19 Treatment Guidelines. [cited 2022 Nov 9]. Available from: https://www.covid19treatmentguidelines.nih.gov/therapies/anti-sars-cov-2-antibody-products/summary-recommendations/
NIH. Pregnancy [Internet]. COVID-19 Treatment Guidelines. [cited 2022 Nov 16]. Available from: https://www.covid19treatmentguidelines.nih.gov/special-populations/pregnancy/
Oaklander AL, Mills AJ, Kelley M, Toran LS, Smith B, Dalakas MC, et al. Peripheral Neuropathy Evaluations of Patients With Prolonged Long COVID. Neurology – Neuroimmunology Neuroinflammation [Internet]. 2022 May 1 [cited 2022 Mar 6];9(3). Available from: https://nn.neurology.org/content/9/3/e1146
Ormiston CK, Świątkiewicz I, Taub PR. Postural orthostatic tachycardia syndrome as a sequela of COVID-19. Heart Rhythm. 2022 Nov;19(11):1880–9. https://doi.org/10.1016/j.hrthm.2022.07.014
Paul BD, Lemle MD, Komaroff AL, Snyder SH. Redox imbalance links COVID-19 and myalgic encephalomyelitis/chronic fatigue syndrome. Proceedings of the National Academy of Sciences. 2021 Aug 24;118(34):e2024358118. https://doi.org/10.1073/pnas.2024358118
Pfaff ER, Madlock-Brown C, Baratta JM, Bhatia A, Davis H, Girvin A, et al. Coding long COVID: characterizing a new disease through an ICD-10 lens. BMC Medicine. 2023 Feb 16;21(1):58. https://doi.org/10.1186/s12916-023-02737-6
Reiken S, Sittenfeld L, Dridi H, Liu Y, Liu X, Marks AR. Alzheimer’s-like signaling in brains of COVID-19 patients. Alzheimer’s & Dementia. 2022;18(5):955–65. https://doi.org/10.1002/alz.12558
Ryan FJ, Hope CM, Masavuli MG, Lynn MA, Mekonnen ZA, Yeow AEL, et al. Long-term perturbation of the peripheral immune system months after SARS-CoV-2 infection. BMC Medicine. 2022 Jan 14;20(1):26. https://doi.org/10.1186/s12916-021-02228-6
SMFM. COVID_treatment_table_6-21-22_(final).pdf [Internet]. [cited 2022 Nov 16]. Available from: https://s3.amazonaws.com/cdn.smfm.org/media/3526/COVID_treatment_table_6-21-22_%28final%29.pdf
Waudby-West R, Parcell BJ, Palmer CNA, Bell S, Chalmers JD, Siddiqui MK. The association between SARS-CoV-2 RT-PCR cycle threshold and mortality in a community cohort. European Respiratory Journal [Internet]. 2021 Jul 1 [cited 2022 Nov 6];58(1). Available from: https://erj.ersjournals.com/content/58/1/2100360
Williams BA, Chamberlain AM, Blankenship JC, Hylek EM, Voyce S. Trends in Atrial Fibrillation Incidence Rates Within an Integrated Health Care Delivery System, 2006 to 2018. JAMA Network Open. 2020 Aug 28;3(8):e2014874. https://doi.org/doi:10.1001/jamanetworkopen.2020.14874
Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med. 2022 Mar;28(3):583–90. https://doi.org/10.1038/s41591-022-01689-3
Yang Z, Wang X, Wang F, Peng Z, Fan Y. A systematic review and meta-analysis of risk factors for intensive care unit acquired weakness. Medicine (Baltimore). 2022 Oct 28;101(43):e31405. https://doi.org/10.1097/MD.0000000000031405
Yong E. Long COVID Has Forced a Reckoning for One of Medicine’s Most Neglected Diseases [Internet]. The Atlantic. 2022 [cited 2022 Oct 14]. Available from: https://www.theatlantic.com/health/archive/2022/09/mecfs-chronic-fatigue-syndrome-doctors-long-covid/671518/
Zhang H, Zang C, Xu Z, Zhang Y, Xu J, Bian J, et al. Data-driven identification of post-acute SARS-CoV-2 infection subphenotypes. Nat Med. 2022 Dec 1;1–10. doi: 10.1038/s41591-022-02116-31
References for “Revenue Cycle Management” presentation
These references are for the presentation “RCM: History, Evolution, Documentation & Coding, and Business Models” presented at the 2023 ASA ADVANCE meeting in Orlando.
- Adams R. UnitedHealthcare Guided Yale’s Groundbreaking Surprise Billing Study [Internet]. The Intercept. 2021 [cited 2021 Aug 15]. Available from: https://theintercept.com/2021/08/10/unitedhealthcare-yale-surprise-billing-study/
- Administrative Consultant Service. Acute Coronary Syndrome DRG Payments [Internet]. Available from: https://www.acsteam.net/sites/acs3/uploads/documents/newsletters/ACSFY17_updated.pdf
- Amadeo K. The Rising Cost of Health Care by Year and Its Causes [Internet]. The Balance. 2022 [cited 2022 Dec 22]. Available from: https://www.thebalancemoney.com/causes-of-rising-healthcare-costs-4064878
- American Diabetes Association. Diagnosis [Internet]. [cited 2021 Aug 31]. Available from: https://www.diabetes.org/a1c/diagnosis
- American Heart Association. Blood Pressure Toolkit [Internet]. [cited 2021 Aug 31]. Available from: https://www.heart.org/en/health-topics/high-blood-pressure/high-blood-pressure-toolkit-resources
- American Medical Association. AMA summary of the interim final rule of the No Surprises Act [Internet]. American Medical Association. [cited 2021 Aug 31]. Available from: https://www.ama-assn.org/delivering-care/patient-support-advocacy/ama-summary-interim-final-rule-no-surprises-act
- Braunwald E, Isselbacher KJ, Petersdorf RG, Wilson JD, Martin JB, Fauci AS. Harrison’s Principles of Internal Medicine. 11th ed. McGraw-Hill Book Company; 1987.
- Burt VL, Whelton P, Roccella EJ, Brown C, Cutler JA, Higgins M, et al. Prevalence of Hypertension in the US Adult Population. Hypertension. 1995 Mar;25(3):305–13.
- Cacace M, Schmid A. The role of diagnosis related groups (DRGs) in healthcare system convergence. BMC Health Services Research. 2009 Nov 5;9(1):A5.
- Carter GM, Newhouse JP, Relles DA. How Much Change in the Case Mix Index is DRG Creep? [Internet]. Rand; 1990 Apr. Available from: https://www.rand.org/content/dam/rand/pubs/reports/2007/R3826.pdf
- Chilingerian J. Origins of DRGs in the United States: A technical, political and cultural story. The Globalization of Managerial Innovation in Health Care. 2008 Jan 1;4–33.
- CMS | History [Internet]. [cited 2021 Jul 31]. Available from: https://www.cms.gov/About-CMS/Agency-Information/History
- CMS. 1995 Documentation Guidelines for Evaluation and Management Services [Internet]. 1995. Available from: https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnedwebguide/downloads/95docguidelines.pdf
- CMS. ICD-10-CM/PCS MS-DRG v37.0 Definitions Manual [Internet]. [cited 2022 Dec 22]. Available from: https://www.cms.gov/icd10m/version37-fullcode-cms/fullcode_cms/P0008.html
- CMS. HHS Announces Rule to Protect Consumers from Surprise Medical Bills [Internet]. [cited 2021 Aug 31]. Available from: https://www.cms.gov/newsroom/press-releases/hhs-announces-rule-protect-consumers-surprise-medical-bills
- https://www.courtlistener.com/docket/13557042/united-states-of-america-v-stanford-healthcare-billing-office/
- Cutting Edge | Medical Billing – Healthcare Analytics [Internet]. [cited 2021 Aug 28]. Available from: https://cuttingedgehca.com/
- Danielsson J. The emperor has no clothes: Limits to risk modelling. Journal of Banking & Finance. 2002 Jul;26(7):1273–96. DOI: 10.1016/S0378-4266(02)00263-7
- DelBene SK. H.R.3173 – 117th Congress (2021-2022): Improving Seniors’ Timely Access to Care Act of 2021 [Internet]. 2022 [cited 2022 Dec 14]. Available from: http://www.congress.gov/
- Donaldson C, Magnussen J. DRGs: The road to hospital efficiency. Health Policy. 1992 May;21(1):47–64.
- Dutton BL, McMenamin P. The Medicare Economic Index: Its Background and Beginnings. Health Care Financ Rev. 1981 Sep;3(1):137–40.
- Ericson C. Is Case Mix Index Still a Relevant Key Performance Indicator? | Journal Of AHIMA [Internet]. 2021 [cited 2021 Aug 29]. Available from: https://journal.ahima.org/is-case-mix-index-still-a-relevant-key-performance-indicator/
- Glance LG, Thirukumaran CP, Feng C, Lustik SJ, Dick AW. Association Between the Physician Quality Score in the Merit-Based Incentive Payment System and Hospital Performance in Hospital Compare in the First Year of the Program. JAMA Network Open. 2021 Aug 3;4(8):e2118449–e2118449.
- Goodhart C. Problems of monetary management : the U.K. experience. Papers in monetary economics 1975 ; 1. 1975;1-20.
- Gorke J. Physician Documentation And Coding: The Third Rail? [Internet]. Forbes. 2019 [cited 2021 Aug 15]. Available from: https://www.forbes.com/sites/jeffgorke/2019/10/24/physician-documentation-and-coding-the-third-rail/
- Grant KB. You Might Want to Get a Second Opinion Before Paying That Medical Bill [Internet]. NBC News. [cited 2021 Aug 31]. Available from: https://www.nbcnews.com/business/consumer/it-s-time-get-second-opinion-paying-medical-bill-n545626
- Hall MA, Schneider CE. Learning from the Legal History of Billing for Medical Fees. J Gen Intern Med. 2008 Aug;23(8):1257–60.
- Hall MA. Making Sense of Referral Fee Statutes. Journal of Health Politics, Policy and Law. 1988 Aug 1;13(4):623–33.
- Juarez G. Non-Profit Taxpayers Against Fraud Urges the Federal Court to Rule Against Stanford Hospital for $468 Million Alleged Healthcare Billing Fraud [Internet]. PR.com. [cited 2021 Aug 9]. Available from: https://www.pr.com/press-release/838884
- Kempker JA, Martin GS. Does Sepsis Case Mix Heterogeneity Prevent Outcome Comparisons? Critical Care Medicine. 2016 Dec;44(12):2288–9.
- Kirkland EB, Heincelman M, Bishu KG, Schumann SO, Schreiner A, Axon RN, et al. Trends in Healthcare Expenditures Among US Adults With Hypertension: National Estimates, 2003–2014. Journal of the American Heart Association. 7(11):e008731. https://doi.org/10.1161/JAHA.118.008731
- Kliff S, Katz J, Taylor R. Hospitals and Insurers Didn’t Want You to See These Prices. Here’s Why. The New York Times [Internet]. 2021 Aug 22 [cited 2021 Aug 25]; Available from: https://www.nytimes.com/interactive/2021/08/22/upshot/hospital-prices.html
- Lagasse J. TeamHealth wins lawsuit against UnitedHealth [Internet]. Healthcare Finance News. 2021 [cited 2022 Dec 24]. Available from: https://www.healthcarefinancenews.com/news/teamhealth-wins-lawsuit-against-unitedhealth
- LaPointe J. Judge Approves Sutter Health’s $575M Antitrust Settlement [Internet]. RevCycleIntelligence. 2021 [cited 2021 Aug 31]. Available from: https://revcycleintelligence.com/news/judge-approves-sutter-healths-575m-antitrust-settlement
- Liang F-W, Wang L-Y, Liu L-Y, Li CY, Lu T-H. Physician code creep after the initiation of outpatient volume control program and implications for appropriate ICD-10-CM coding. BMC Health Services Research. 2020 Feb 19;20(1):127.
- Liss S. Texas judge throws out piece of surprise billing rule in win for providers [Internet]. Healthcare Dive. 2022 [cited 2023 Jan 12]. Available from: https://www.healthcaredive.com/news/texas-judge-strikes-down-part-surprise-billing-rule/619357/
- Liss S. Judge questions surprise billing ban implementation during court hearing [Internet]. Healthcare Dive. 2022 [cited 2022 Dec 23]. Available from: https://www.healthcaredive.com/news/judge-questions-surprise-billing-ban-implementation/639206/
- Liu J, Capurro D, Nguyen A, Verspoor K. Early prediction of diagnostic-related groups and estimation of hospital cost by processing clinical notes. npj Digit Med. 2021 Jul 1;4(1):1–8. https://www.nature.com/articles/s41746-021-00474-9
- Loscalzo J, Fauci AS, Kasper DL, Hauser SL, Longo DL, Jameson JL. Harrison’s Principles of Internal Medicine. 21st ed. McGraw-Hill / Medical; 2022.
- Lundeen JM, Souba WW, Hollenbeak CS. Sources of Error in Delayed Payment of Physician Claims. Family Medicine. 2003 May;35(5):355–9.
- Medical Practice Partners. Revenue Cycle Management [Internet]. [cited 2021 Aug 28]. Available from: https://www.medicalpracticepartners.com/
- Morse S. CMS releases Advancing Interoperability and Improving Prior Authorization Processes Proposed Rule [Internet]. Healthcare Finance News. [cited 2022 Dec 13]. Available from: https://www.healthcarefinancenews.com/news/cms-releases-advancing-interoperability-and-improving-prior-authorization-processes-proposed
- Morse S. UnitedHealth sues TeamHealth, saying it overpaid $100 million in claims [Internet]. Healthcare Finance News. 2021 [cited 2023 Jan 12]. Available from: https://www.healthcarefinancenews.com/news/unitedhealth-sues-teamhealth-saying-it-overpaid-100-million-claims
- Muntner P, Miles MA, Jaeger BC, Hannon III L, Hardy ST, Ostchega Y, et al. Blood Pressure Control Among US Adults, 2009 to 2012 Through 2017 to 2020. Hypertension. 2022 Sep;79(9):1971–80. https://doi.org/10.1161/HYPERTENSIONAHA.122.19222
- Muoio, Dave. “Damning assessment” finds few ties between physicians’ MIPS scores and stronger surgical outcomes [Internet]. FierceHealthcare. [cited 2021 Aug 9]. Available from: https://www.fiercehealthcare.com/practices/damning-assessment-finds-few-ties-between-physicians-mips-scores-and-stronger-surgical
- The History of Medicare [Internet]. National Academy of Social Insurance. [cited 2022 Dec 22]. Available from: https://www.nasi.org/learn/medicare/the-history-of-medicare/
- OIG. Improper Payments for Evaluation and Management Services Cost Medicare Billions in 2010 (OEI-04-10-00181; 05/14). 2014 May;(OEI-04-10-00181):44.
- OIG. Medicare Hospital Prospective Payment System [Internet]. OIG; 2001 Aug [cited 2021 Aug 25]. Report No.: OEI-09-00-00200. Available from: https://oig.hhs.gov/oei/reports/oei-09-00-00200.pdf
- Ostrov BF. Fallout from A Failed Health Insurer [Internet]. Center for Health Journalism. [cited 2022 Dec 14]. Available from: https://centerforhealthjournalism.org/fellowships/projects/fallout-failed-health-insurer
- Pallardy, Carrie. 90% of Solo, Small Physician Practices Plan to Outsource Medical Billing [Internet]. [cited 2021 Aug 15]. Available from: https://www.beckersasc.com/asc-coding-billing-and-collections/90-of-solo-small-physician-practices-plan-to-outsource-medical-billing.html?oly_enc_id=1683B3235756H4V
- Pallone F. Text – H.R.3630 – 116th Congress (2019-2020): No Surprises Act [Internet]. 2019 [cited 2021 Aug 31]. Available from: https://www.congress.gov/bill/116th-congress/house-bill/3630/text
- Parris R, Schoenvogel M. The Art of Putting It Together [Internet]. Huron Healthcare (Huron Consulting Group); Available from: http://www.huronconsultinggroup.com/~/media/Resource%20Media%20Content/Healthcare/151566%20Print%20Healthcare_WP_RC_ConsolidationStandardization_Final
- Pauker KY. A History of RBRVS as a Perspective on P4P — Part I. CSA Bulletin. 2006;(Spring):7.
- Pestaina K, Pollitz K. Examining Prior Authorization in Health Insurance [Internet]. KFF. 2022 [cited 2022 Dec 14]. Available from: https://www.kff.org/policy-watch/examining-prior-authorization-in-health-insurance/
- Pettengill J, Vertrees J. Reliability and Validity in Hospital Case-Mix Measurement. Health Care Financ Rev. 1982 Dec;4(2):101–28.
- Plawecki AM, Singer MC, Peterson EL, Yaremchuk KL. Impact of a specialty trained billing team on an academic otolaryngology practcice. American Journal of Otolaryngology. 2020 Sep;41.
- Pollitz K, Jan 20 DMP, 2021. Claims Denials and Appeals in ACA Marketplace Plans [Internet]. KFF. 2021 [cited 2021 Aug 31]. Available from: https://www.kff.org/private-insurance/issue-brief/claims-denials-and-appeals-in-aca-marketplace-plans/
- Quantin C, Sauleau E, Bolard P, Mousson C, Kerkri M, Lecomte PB, et al. Modeling of High-cost Patient Distribution within Renal Failure Diagnosis Related Group. Journal of Clinical Epidemiology. 1999 Mar;52(3):251–8.
- Reddy P. Special General Medical Staff Meeting. 2014 Dec 2; O’Connor Hospital, San Jose, CA.
- Román P, Ruiz-Cantero A. Polypathology, an emerging phenomenon and a challenge for healthcare systems. Revista Clínica Española (English Edition). 2017 May;217(4):229–37.
- Rosenthal E. How health insurance changed from protecting patients to seeking profit [Internet]. Stanford Medicine. [cited 2021 Aug 13]. Available from: http://stanmed.stanford.edu/2017spring/how-health-insurance-changed-from-protecting-patients-to-seeking-profit.html
- Russo R. Documentation and Data Improvement Fundamentals. Documentation and Data Improvement Fundamentals / AHIMA, American Health Information Management Association [Internet]. 2004 Oct 15 [cited 2021 Aug 15]; Available from: http://library.ahima.org/doc?oid=60174
- Schulte F, Fry E. Death By 1,000 Clicks: Where Electronic Health Records Went Wrong [Internet]. Kaiser Health News. 2019 [cited 2022 Dec 14]. Available from: https://khn.org/news/death-by-a-thousand-clicks/
- Schwartz K, Lopez E, 2020. What We Know About Provider Consolidation [Internet]. KFF. 2020 [cited 2021 Aug 31]. Available from: https://www.kff.org/health-costs/issue-brief/what-we-know-about-provider-consolidation/
- Shafrin J. What is the difference between DRGs, AP-DRGs, and APR-DRGs? – Healthcare Economist [Internet]. 2012 [cited 2022 Dec 27]. Available from: https://www.healthcare-economist.com/2012/06/19/what-is-the-difference-between-drgs-ap-drgs-and-apr-drgs/
- Shankar-Hari M, Harrison D, Rowan K. Differences in Impact of Definitional Elements on Mortality Precludes International Comparisons of Sepsis Epidemiology. Crit Care Med. 2016 Dec;44(12):2223–30.
- Simborg D. DRG Creep: a new hospital-acquired disease. New England Journal of Medicine. 1981 Jun 25; 304(26):1602-1604.
- Sjoding MW, Iwashyna TJ, Dimick JB, Cooke CR. Gaming Hospital-Level Pneumonia 30-Day Mortality and Readmission Measures by Legitimate Changes to Diagnostic Coding*. Critical Care Medicine. 2015 May;43(5):989–95.
- Slade E, Tamber PS, Vincent J-L. The Surviving Sepsis Campaign: raising awareness to reduce mortality. Crit Care. 2003 Jan 8;7(1):1.
- Society of Critical Care Medicine. Surviving Sepsis Campaign (SSC) [Internet]. [cited 2021 Aug 29]. Available from: https://www.sccm.org/SurvivingSepsisCampaign/Home
- Steinwald B, Dummit LA. Hospital Case-Mix Change: Sicker Patients Or Drg Creep? Health Affairs. 1989 Jan 1;8(2):35–47.
- Technavio. $ 27.43 Billion Growth in Global Healthcare Revenue Cycle Management (RCM) Software Market 2021-2025 | Featuring 3M Co., Allscripts Healthcare Solutions Inc., and Change Healthcare Inc. among others | Technavio [Internet]. [cited 2021 Jul 28]. Available from: https://www.prnewswire.com/news-releases/-27-43-billion-growth-in-global-healthcare-revenue-cycle-management-rcm-software-market-2021-2025–featuring-3m-co-allscripts-healthcare-solutions-inc-and-change-healthcare-inc-among-others–technavio-301256263.html
- Tinetti ME, Fried TR, Boyd CM. Designing Health Care for the Most Common Chronic Condition—Multimorbidity. JAMA. 2012 Jun 20;307(23):2493–4.
- UFCW v. Sutter Health – Home [Internet]. [cited 2021 Aug 31]. Available from: https://www.sutterhealthlawsuit.com/
- United States v. Stanford Healthcare Billing Department. United States District Court, Northern District of California. Case 17-CV-08726-DSF-AFM.
- US Department of Justice. Prime Healthcare Services and CEO to Pay $65 Million to Settle False Claims Act Allegations [Internet]. 2018 [cited 2021 Aug 29]. Available from: https://www.justice.gov/opa/pr/prime-healthcare-services-and-ceo-pay-65-million-settle-false-claims-act-allegations
- US Department of Justice. Prime Healthcare Services and Two Doctors Agree to Pay $37.5 Million to Settle Allegations of Kickbacks, Billing for a Suspended Doctor, and False Claims for Implantable Medical Hardware [Internet]. 2021 [cited 2021 Aug 10]. Available from: https://www.justice.gov/opa/pr/prime-healthcare-services-and-two-doctors-agree-pay-375-million-settle-allegations-kickbacks
- US Department of Justice. Sutter Health and Affiliates to Pay $90 Million to Settle False Claims Act Allegations of Mischarging the Medicare Advantage Program [Internet]. 2021 [cited 2021 Aug 31]. Available from: https://www.justice.gov/opa/pr/sutter-health-and-affiliates-pay-90-million-settle-false-claims-act-allegations-mischarging
- Wei MY, Luster JE, Chan C-L, Min L. Comprehensive review of ICD-9 code accuracies to measure multimorbidity in administrative data. BMC Health Services Research. 2020 Jun 1;20(1):489.